Tuesday Poster Session
Category: Biliary/Pancreas
P3538 - Autoimmune Pancreatitis Presenting as Multifocal Masses: A Rare Presentation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Aqsa Khan, MD
Parkview Health Center
Fort Wayne, IN
Presenting Author(s)
Aqsa Khan, MD1, Neil R. Sharma, MD2
1Parkview Health Center, Fort Wayne, IN; 2Peak Gastroenterolgy, Colorado Springs, CO
Introduction: Autoimmune pancreatitis is a rare and benign condition that at times can mimic pancreatic cancer both clinically and radiologically. There are two types of AIP. Type 1 AIP is a systemic disorder, and is usually associated with elevated levels of systemic IgG4 whereas type 2 AIP is primary pancreatic disorder and not associated with IgG4 positive cells. We present a case of 64-year-old female who was found to have submandibular and anterior cervical lymphadenopathy on routine physical examination and lead to the diagnosis of AIP
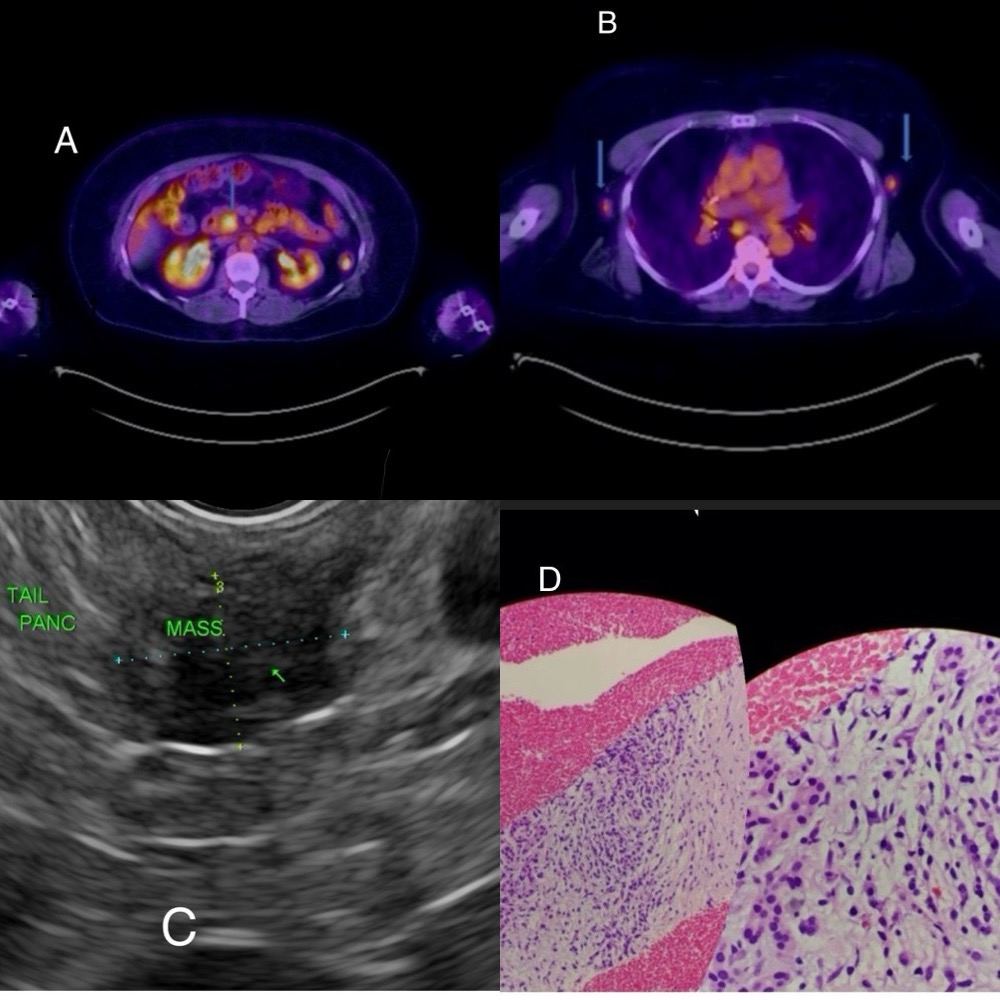
Case Description/Methods: 64-year-old female with history of COPD was found to have anterior cervical and submandibular lymphadenopathy during a routine physical examination. TB skin test was negative. CT scan of the neck without contrast showed enlarged bilateral parotid and submandibular glands with innumerable lymph nodes. CT chest showed several mediastinal lymph nodes. To look for the source of lymphadenopathy, PET/CT was obtained which showed focal FDG activity within pancreas or adjacent to it. Other findings included FDG avid lymph nodes in the neck, chest and abdomen concerning metastatic disease.
Excisional biopsy of upper left neck mass was done, and pathology was compatible with IgG4 related sialadenitis. The CT abdomen Triphasic pancreas with and without contrast showed contour of pancreas preserved, no masses seen. Endoscopic ultrasound (EUS) with FNB (core biopsy) was done for the diagnosis and to rule out malignancy.
EUS showed multifocal pancreatic masses at three sites. Biopsies were taken and final pathology revealed type 1 autoimmune pancreatitis with no evidence of malignancy. Pancreatic tail biopsy showed changes consistent with autoimmune pancreatitis including storiform fibrosis, increased number of IgG4-positive cells, lymphoplasmacytic inflammation, and obliterative phlebitis. No evidence of malignancy.
Patient was started on Prednisone 40 mg and on follow up exam in 3 months a repeat CT Abdomen/ Pelvis and CT Chest was negative for any acute pathology.
Discussion: Autoimmune pancreatitis rarely presents with multifocal masses which could be confused with
pancreatic cancer or pancreatic metastasis. Patients may not always present with typical clinical
features of AIP like obstructive jaundice or abdominal pain. AIP responds very well to
corticosteroids. Treatment results in resolution of autoimmune pancreatitis findings and
symptoms. Extra pancreatic findings also respond to steroids in autoimmune pancreatitis.
Disclosures:
Aqsa Khan, MD1, Neil R. Sharma, MD2. P3538 - Autoimmune Pancreatitis Presenting as Multifocal Masses: A Rare Presentation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Parkview Health Center, Fort Wayne, IN; 2Peak Gastroenterolgy, Colorado Springs, CO
Introduction: Autoimmune pancreatitis is a rare and benign condition that at times can mimic pancreatic cancer both clinically and radiologically. There are two types of AIP. Type 1 AIP is a systemic disorder, and is usually associated with elevated levels of systemic IgG4 whereas type 2 AIP is primary pancreatic disorder and not associated with IgG4 positive cells. We present a case of 64-year-old female who was found to have submandibular and anterior cervical lymphadenopathy on routine physical examination and lead to the diagnosis of AIP
Case Description/Methods: 64-year-old female with history of COPD was found to have anterior cervical and submandibular lymphadenopathy during a routine physical examination. TB skin test was negative. CT scan of the neck without contrast showed enlarged bilateral parotid and submandibular glands with innumerable lymph nodes. CT chest showed several mediastinal lymph nodes. To look for the source of lymphadenopathy, PET/CT was obtained which showed focal FDG activity within pancreas or adjacent to it. Other findings included FDG avid lymph nodes in the neck, chest and abdomen concerning metastatic disease.
Excisional biopsy of upper left neck mass was done, and pathology was compatible with IgG4 related sialadenitis. The CT abdomen Triphasic pancreas with and without contrast showed contour of pancreas preserved, no masses seen. Endoscopic ultrasound (EUS) with FNB (core biopsy) was done for the diagnosis and to rule out malignancy.
EUS showed multifocal pancreatic masses at three sites. Biopsies were taken and final pathology revealed type 1 autoimmune pancreatitis with no evidence of malignancy. Pancreatic tail biopsy showed changes consistent with autoimmune pancreatitis including storiform fibrosis, increased number of IgG4-positive cells, lymphoplasmacytic inflammation, and obliterative phlebitis. No evidence of malignancy.
Patient was started on Prednisone 40 mg and on follow up exam in 3 months a repeat CT Abdomen/ Pelvis and CT Chest was negative for any acute pathology.
Discussion: Autoimmune pancreatitis rarely presents with multifocal masses which could be confused with
pancreatic cancer or pancreatic metastasis. Patients may not always present with typical clinical
features of AIP like obstructive jaundice or abdominal pain. AIP responds very well to
corticosteroids. Treatment results in resolution of autoimmune pancreatitis findings and
symptoms. Extra pancreatic findings also respond to steroids in autoimmune pancreatitis.
Figure: A and B showing FGD activity in Pancreas and axillary lymph nodes
C: EUS showing masses in pancreas
D: Pathology showing Plasma Cells
C: EUS showing masses in pancreas
D: Pathology showing Plasma Cells
Disclosures:
Aqsa Khan indicated no relevant financial relationships.
Neil R. Sharma indicated no relevant financial relationships.
Aqsa Khan, MD1, Neil R. Sharma, MD2. P3538 - Autoimmune Pancreatitis Presenting as Multifocal Masses: A Rare Presentation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
