Tuesday Poster Session
Category: Biliary/Pancreas
P3540 - A Trail of Blood: Exploring a Rare Cause of Pancreatic Bleeding
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Fady Gendy, DO
Geisinger Health System
Danville, PA
Presenting Author(s)
Fady Gendy, DO1, Deepa S. Kumarjiguda, DO2, Michael Makar, MD1, Ashok Bhanushali, MD1, David L. Diehl, MD1, Bradley D.. Confer, DO1, Dema Shamoon, MD1
1Geisinger Health System, Danville, PA; 2Geisinger Medical Center, Danville, PA
Introduction: Hemosuccus Pancreaticus (HP) is a rare cause of upper gastrointestinal (GI) bleeding in which a vascular malformation creates an anastomosis into the pancreatic duct, causing massive hemorrhage. Acute or chronic pancreatitis can be responsible for up to 80% of cases of HP, due to subsequent vascular wall rupture. HP can also be seen in the setting of arterial aneurysms such as the case that will be discussed in this report.
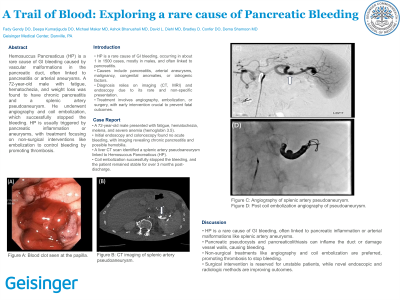
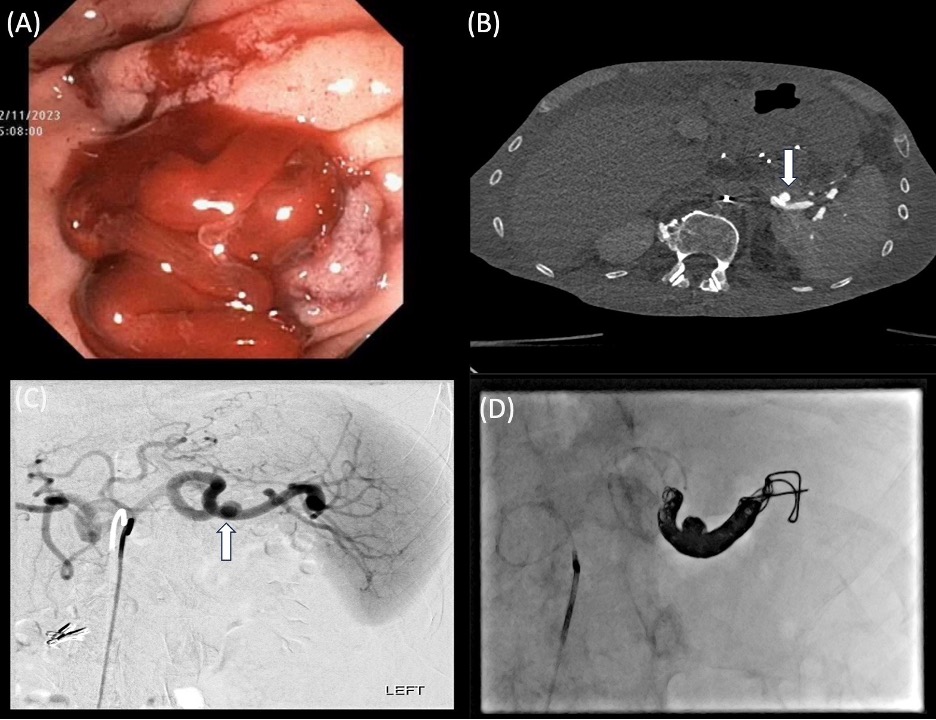
Case Description/Methods: A 72-year old male presented to the hospital with fatigue, hematochezia, melena, and weight loss for about a week. When he arrived at the hospital, he was found to be profoundly anemic with hemoglobin of 3.5. Computer tomography (CT) imaging of his abdomen revealed chronic pancreatitis but no cause of acute bleeding. A duodenal scope was utilized which did not reveal any sign of acute bleeding but did reveal some scant blood in the duodenum concerning for possible hemobilia (figure A). A three-phase liver CT scan was done, which revealed a splenic artery pseudoaneurysm extending into the tail of the pancreas concerning for HP (figure B). The patient immediately underwent angiography and coil embolization of the pseudoaneurysm (figure C & D). After the procedure, the patient’s melena and hematochezia stopped and he had no further episodes of bleeding. He remained hemodynamically stable continued to be after over 3 months of outpatient follow-up.
Discussion: HP is an extremely rare cause of GI bleeding usually caused by pancreatic inflammation or vascular malformation, which were both seen in this patient’s case. Pancreatic inflammation can cause HP through rupture of a peripheral vascular wall, but also through pancreaticolithiasis and pseudocysts which can inflame the pancreatic duct. Arterial malformations can also cause HP with aneurysms or pseudoaneurysms of the splenic artery being most common.
The treatment of HP focuses on addressing the source of bleeding. Generally, non-surgical approaches are taken for hemodynamically stable patients, which consist of angiography and embolization as demonstrated in this case. Coil embolization ultimately stimulates thrombosis within the vascular malformation and stops the bleeding. Novel approaches have utilized metal arterial stents and lipidol/histoacryl mixtures to stop the bleeding with promising results. Ultimately, once HP is properly diagnosed and addressed, patients generally have good outcomes.
Disclosures:
Fady Gendy, DO1, Deepa S. Kumarjiguda, DO2, Michael Makar, MD1, Ashok Bhanushali, MD1, David L. Diehl, MD1, Bradley D.. Confer, DO1, Dema Shamoon, MD1. P3540 - A Trail of Blood: Exploring a Rare Cause of Pancreatic Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Geisinger Health System, Danville, PA; 2Geisinger Medical Center, Danville, PA
Introduction: Hemosuccus Pancreaticus (HP) is a rare cause of upper gastrointestinal (GI) bleeding in which a vascular malformation creates an anastomosis into the pancreatic duct, causing massive hemorrhage. Acute or chronic pancreatitis can be responsible for up to 80% of cases of HP, due to subsequent vascular wall rupture. HP can also be seen in the setting of arterial aneurysms such as the case that will be discussed in this report.
Case Description/Methods: A 72-year old male presented to the hospital with fatigue, hematochezia, melena, and weight loss for about a week. When he arrived at the hospital, he was found to be profoundly anemic with hemoglobin of 3.5. Computer tomography (CT) imaging of his abdomen revealed chronic pancreatitis but no cause of acute bleeding. A duodenal scope was utilized which did not reveal any sign of acute bleeding but did reveal some scant blood in the duodenum concerning for possible hemobilia (figure A). A three-phase liver CT scan was done, which revealed a splenic artery pseudoaneurysm extending into the tail of the pancreas concerning for HP (figure B). The patient immediately underwent angiography and coil embolization of the pseudoaneurysm (figure C & D). After the procedure, the patient’s melena and hematochezia stopped and he had no further episodes of bleeding. He remained hemodynamically stable continued to be after over 3 months of outpatient follow-up.
Discussion: HP is an extremely rare cause of GI bleeding usually caused by pancreatic inflammation or vascular malformation, which were both seen in this patient’s case. Pancreatic inflammation can cause HP through rupture of a peripheral vascular wall, but also through pancreaticolithiasis and pseudocysts which can inflame the pancreatic duct. Arterial malformations can also cause HP with aneurysms or pseudoaneurysms of the splenic artery being most common.
The treatment of HP focuses on addressing the source of bleeding. Generally, non-surgical approaches are taken for hemodynamically stable patients, which consist of angiography and embolization as demonstrated in this case. Coil embolization ultimately stimulates thrombosis within the vascular malformation and stops the bleeding. Novel approaches have utilized metal arterial stents and lipidol/histoacryl mixtures to stop the bleeding with promising results. Ultimately, once HP is properly diagnosed and addressed, patients generally have good outcomes.
Figure: A: Blood clot seen at the papilla.
B: CT imaging of splenic artery pseudoaneurysm.
C: Angiography of splenic artery pseudoaneurysm.
D: Post coil embolization angiography of pseudoaneurysm.
B: CT imaging of splenic artery pseudoaneurysm.
C: Angiography of splenic artery pseudoaneurysm.
D: Post coil embolization angiography of pseudoaneurysm.
Disclosures:
Fady Gendy indicated no relevant financial relationships.
Deepa Kumarjiguda indicated no relevant financial relationships.
Michael Makar indicated no relevant financial relationships.
Ashok Bhanushali indicated no relevant financial relationships.
David Diehl: Castle Biosciences – Consultant.
Bradley Confer: Boston Scientific Corporation – Consultant. Exact Sciences – Advisory Committee/Board Member, FDA advisory panel.
Dema Shamoon indicated no relevant financial relationships.
Fady Gendy, DO1, Deepa S. Kumarjiguda, DO2, Michael Makar, MD1, Ashok Bhanushali, MD1, David L. Diehl, MD1, Bradley D.. Confer, DO1, Dema Shamoon, MD1. P3540 - A Trail of Blood: Exploring a Rare Cause of Pancreatic Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
