Tuesday Poster Session
Category: Biliary/Pancreas
P3545 - Recurrence of Intraductal Papillary Mucinous Neoplasm Leading to Aggressive Metastatic Pancreatic Cancer Post-Frey Procedure: A Case Study and Role of Interventional Endoscopy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Fnu Vikash, MD, M.Med
Albert Einstein College of Medicine
New York, NY
Presenting Author(s)
Fnu Vikash, MD, M.Med1, Nicholas Costable, MD2, Gautam Maddineni, MD3, Ahan Bhatt, MD1, Sindhu Vikash, MD4, Vikash Kumar, MD5, Abu Fahad Abbasi, MD6, Sammy Ho, MD, FACG7
1Albert Einstein College of Medicine, New York, NY; 2Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 3Florida State University, Cape Coral, FL; 4Cleveland Clinic, Bronx, NY; 5Creighton University School of Medicine, Brooklyn, NY; 6Mercy Health, Rockford, IL; 7Montefiore Medical Center, New York, NY
Introduction: The prognosis of intraductal papillary‑mucinous neoplasm (IPMN) is superior to pancreatic ductal adenocarcinoma (PDAC). To date, only a limited number of advanced cases of IPMN have been documented. We present a first case in the US where IPMN recurred as metastatic PDAC, emerging seven months after the Frey procedure.
Case Description/Methods: A 57-year-old male smoker with a history of uncontrolled type 2 diabetes presented to the ED with epigastric pain for 2 days. Physical examination revealed epigastric tenderness. Laboratory results showed normal CBC, elevated ALT 222, AST 149, ALP 675, T.Bili 2.6, D.Bili 2.0, and lipase 460. CT scan was consistent with acute pancreatitis (AP) and a 4.3 cm cystic mass in pancreatic head concerning pancreatic pseudocyst, with common bile and pancreatic duct dilation.
Despite undergoing ERCP with sphincterotomy, the patient had recurrent hospitalizations for similar complaints over the past year. Subsequently, the patient had a Frey procedure. A pancreatic excision biopsy confirmed the presence of IPMN with high-grade dysplasia and no evidence of invasive carcinoma in the specimen. Despite interventions, abdominal pain persisted, leading to multiple hospitalizations over the next seven months. Subsequently, an abdominal MRI revealed a 6 mm T2 hyperintense focus in the superior right hepatic lobe and thrombosis in the portal, mesenteric, and splenic veins. Eliquis was initiated.
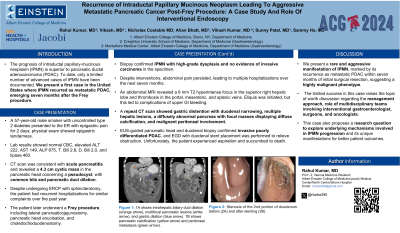
A repeat CT scan showed gastric distention with duodenal narrowing, multiple hepatic lesions, diffusely abnormal pancreas with focal masses displaying diffuse calcification, and malignant peritoneal involvement (Figure 1). EUS-guided pancreatic head and duodenal biopsy confirmed invasive poorly differentiated PDAC and EGD with duodenal stent was performed to relieve the obstruction (Figure 2). Unfortunately, the patient aspirated was arrested and succumbed to death.
Discussion: We present a rare and aggressive manifestation of IPMN, marked by its recurrence as metastatic PDAC within seven months of initial surgical resection, suggesting a highly malignant phenotype. The limited success in this case raises the topic of worth discussion regarding the management approach and role of multidisciplinary teams involving interventional gastroenterologists, surgeons, and oncologists. This case also proposes a research question to explore the underlying mechanisms involved in IPMN progression and its unique manifestations for better patient outcomes.

Disclosures:
Fnu Vikash, MD, M.Med1, Nicholas Costable, MD2, Gautam Maddineni, MD3, Ahan Bhatt, MD1, Sindhu Vikash, MD4, Vikash Kumar, MD5, Abu Fahad Abbasi, MD6, Sammy Ho, MD, FACG7. P3545 - Recurrence of Intraductal Papillary Mucinous Neoplasm Leading to Aggressive Metastatic Pancreatic Cancer Post-Frey Procedure: A Case Study and Role of Interventional Endoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein College of Medicine, New York, NY; 2Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 3Florida State University, Cape Coral, FL; 4Cleveland Clinic, Bronx, NY; 5Creighton University School of Medicine, Brooklyn, NY; 6Mercy Health, Rockford, IL; 7Montefiore Medical Center, New York, NY
Introduction: The prognosis of intraductal papillary‑mucinous neoplasm (IPMN) is superior to pancreatic ductal adenocarcinoma (PDAC). To date, only a limited number of advanced cases of IPMN have been documented. We present a first case in the US where IPMN recurred as metastatic PDAC, emerging seven months after the Frey procedure.
Case Description/Methods: A 57-year-old male smoker with a history of uncontrolled type 2 diabetes presented to the ED with epigastric pain for 2 days. Physical examination revealed epigastric tenderness. Laboratory results showed normal CBC, elevated ALT 222, AST 149, ALP 675, T.Bili 2.6, D.Bili 2.0, and lipase 460. CT scan was consistent with acute pancreatitis (AP) and a 4.3 cm cystic mass in pancreatic head concerning pancreatic pseudocyst, with common bile and pancreatic duct dilation.
Despite undergoing ERCP with sphincterotomy, the patient had recurrent hospitalizations for similar complaints over the past year. Subsequently, the patient had a Frey procedure. A pancreatic excision biopsy confirmed the presence of IPMN with high-grade dysplasia and no evidence of invasive carcinoma in the specimen. Despite interventions, abdominal pain persisted, leading to multiple hospitalizations over the next seven months. Subsequently, an abdominal MRI revealed a 6 mm T2 hyperintense focus in the superior right hepatic lobe and thrombosis in the portal, mesenteric, and splenic veins. Eliquis was initiated.
A repeat CT scan showed gastric distention with duodenal narrowing, multiple hepatic lesions, diffusely abnormal pancreas with focal masses displaying diffuse calcification, and malignant peritoneal involvement (Figure 1). EUS-guided pancreatic head and duodenal biopsy confirmed invasive poorly differentiated PDAC and EGD with duodenal stent was performed to relieve the obstruction (Figure 2). Unfortunately, the patient aspirated was arrested and succumbed to death.
Discussion: We present a rare and aggressive manifestation of IPMN, marked by its recurrence as metastatic PDAC within seven months of initial surgical resection, suggesting a highly malignant phenotype. The limited success in this case raises the topic of worth discussion regarding the management approach and role of multidisciplinary teams involving interventional gastroenterologists, surgeons, and oncologists. This case also proposes a research question to explore the underlying mechanisms involved in IPMN progression and its unique manifestations for better patient outcomes.

Figure: Figure 1 & 2
Disclosures:
Fnu Vikash indicated no relevant financial relationships.
Nicholas Costable indicated no relevant financial relationships.
Gautam Maddineni indicated no relevant financial relationships.
Ahan Bhatt indicated no relevant financial relationships.
Sindhu Vikash indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Abu Fahad Abbasi indicated no relevant financial relationships.
Sammy Ho indicated no relevant financial relationships.
Fnu Vikash, MD, M.Med1, Nicholas Costable, MD2, Gautam Maddineni, MD3, Ahan Bhatt, MD1, Sindhu Vikash, MD4, Vikash Kumar, MD5, Abu Fahad Abbasi, MD6, Sammy Ho, MD, FACG7. P3545 - Recurrence of Intraductal Papillary Mucinous Neoplasm Leading to Aggressive Metastatic Pancreatic Cancer Post-Frey Procedure: A Case Study and Role of Interventional Endoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

