Tuesday Poster Session
Category: Biliary/Pancreas
P3546 - Dead End! Iatrogenic Bile Duct Injury and a Successful Salvage!
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Ahmad Abulawi, MD
Albany Medical College
Albany, NY
Presenting Author(s)
Ahmad Abulawi, MD, Stephen Hasak, MD, MPH
Albany Medical College, Albany, NY
Introduction: Bile duct injury (BDI) remains the most serious and life-threatening complication of cholecystectomy (CCY). Since the introduction of laparoscopic cholecystectomy (LC) in 1987, the incidence of iatrogenic injuries has increased worldwide. Here, we present a serious case of iatrogenic bile duct obstruction during CCY.
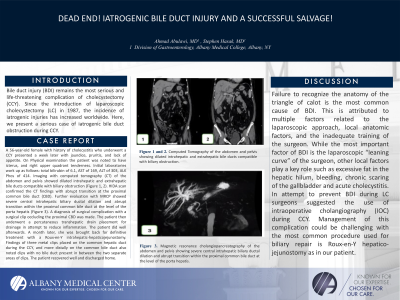
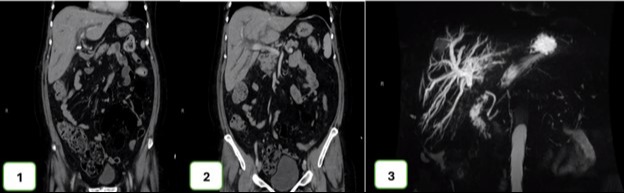
Case Description/Methods: A 56-year-old female with history of cholecystitis who underwent a CCY presented a week later with jaundice, pruritis, and lack of appetite. On Physical examination the patient was noted to have icterus, and right upper quadrant tenderness. Initial laboratories work up as follows: total bilirubin of 6.1, AST of 169, ALT of 303, ALK Phos of 414. Imaging with computed tomography (CT) of the abdomen and pelvis showed dilated intrahepatic and extrahepatic bile ducts compatible with biliary obstruction (Figure 1, 2). HIDA scan confirmed the CT findings with abrupt transition at the proximal common bile duct (CBD). Further evaluation with MRCP showed severe central intrahepatic biliary ductal dilation and abrupt transition within the proximal common bile duct at the level of the porta hepatis (Figure 3). A diagnosis of surgical complication with a surgical clip occluding the proximal CBD was made. The patient then underwent a percutaneous transhepatic drain placement for drainage in attempt to reduce inflammation. The patient did well afterwards. A month later, she was brought back for definitive treatment with a Roux-en-Y intrahepatic-hepaticojejunostomy. Findings of three metal clips placed on the common hepatic duct during the CCY, and more distally on the common bile duct also noted clips with no bile duct present in between the two separate areas of clips. The patient recovered well and discharged home.
Discussion: Failure to recognize the anatomy of the triangle of calot is the most common cause of BDI. This is attributed to multiple factors related to the laparoscopic approach, local anatomic factors, and the inadequate training of the surgeon. While the most important factor of BDI is the laparoscopic “leaning curve” of the surgeon, other local factors play a key role such as excessive fat in the hepatic hilum, bleeding, chronic scaring of the gallbladder and acute cholecystitis. In attempt to prevent BDI during LC surgeons suggested the use of intraoperative cholangiography (IOC) during CCY. Management of this complication could be challenging with the most common procedure used for biliary repair is Roux-en-Y hepatico-jejunostomy as in our patient.
Disclosures:
Ahmad Abulawi, MD, Stephen Hasak, MD, MPH. P3546 - Dead End! Iatrogenic Bile Duct Injury and a Successful Salvage!, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Albany Medical College, Albany, NY
Introduction: Bile duct injury (BDI) remains the most serious and life-threatening complication of cholecystectomy (CCY). Since the introduction of laparoscopic cholecystectomy (LC) in 1987, the incidence of iatrogenic injuries has increased worldwide. Here, we present a serious case of iatrogenic bile duct obstruction during CCY.
Case Description/Methods: A 56-year-old female with history of cholecystitis who underwent a CCY presented a week later with jaundice, pruritis, and lack of appetite. On Physical examination the patient was noted to have icterus, and right upper quadrant tenderness. Initial laboratories work up as follows: total bilirubin of 6.1, AST of 169, ALT of 303, ALK Phos of 414. Imaging with computed tomography (CT) of the abdomen and pelvis showed dilated intrahepatic and extrahepatic bile ducts compatible with biliary obstruction (Figure 1, 2). HIDA scan confirmed the CT findings with abrupt transition at the proximal common bile duct (CBD). Further evaluation with MRCP showed severe central intrahepatic biliary ductal dilation and abrupt transition within the proximal common bile duct at the level of the porta hepatis (Figure 3). A diagnosis of surgical complication with a surgical clip occluding the proximal CBD was made. The patient then underwent a percutaneous transhepatic drain placement for drainage in attempt to reduce inflammation. The patient did well afterwards. A month later, she was brought back for definitive treatment with a Roux-en-Y intrahepatic-hepaticojejunostomy. Findings of three metal clips placed on the common hepatic duct during the CCY, and more distally on the common bile duct also noted clips with no bile duct present in between the two separate areas of clips. The patient recovered well and discharged home.
Discussion: Failure to recognize the anatomy of the triangle of calot is the most common cause of BDI. This is attributed to multiple factors related to the laparoscopic approach, local anatomic factors, and the inadequate training of the surgeon. While the most important factor of BDI is the laparoscopic “leaning curve” of the surgeon, other local factors play a key role such as excessive fat in the hepatic hilum, bleeding, chronic scaring of the gallbladder and acute cholecystitis. In attempt to prevent BDI during LC surgeons suggested the use of intraoperative cholangiography (IOC) during CCY. Management of this complication could be challenging with the most common procedure used for biliary repair is Roux-en-Y hepatico-jejunostomy as in our patient.
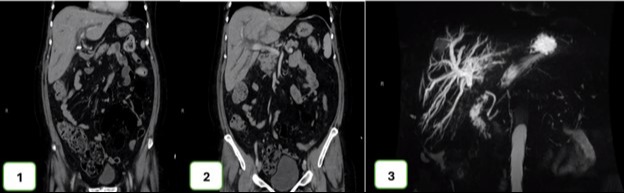
Figure: Figure 1 and 2: Computed Tomography of the abdomen and pelvis showing dilated intrahepatic and extrahepatic bile ducts compatible with biliary obstruction.
Figure 3: Magnetic resonance cholangiopancreatography of the abdomen and pelvis showing severe central intrahepatic biliary ductal dilation and abrupt transition within the proximal common bile duct at the level of the porta hepatis.
Figure 3: Magnetic resonance cholangiopancreatography of the abdomen and pelvis showing severe central intrahepatic biliary ductal dilation and abrupt transition within the proximal common bile duct at the level of the porta hepatis.
Disclosures:
Ahmad Abulawi indicated no relevant financial relationships.
Stephen Hasak indicated no relevant financial relationships.
Ahmad Abulawi, MD, Stephen Hasak, MD, MPH. P3546 - Dead End! Iatrogenic Bile Duct Injury and a Successful Salvage!, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
