Tuesday Poster Session
Category: Biliary/Pancreas
P3550 - A Case of Pancreatic Neuroendocrine Tumor Recurrence and Development of Type 3c diabetes
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Tinsa Varughese, DO
Lehigh Valley Health Network
Allentown, PA
Presenting Author(s)
Tinsa Varughese, DO, Amanda Jacubowsky, DO, Anne Borja, MD, Lindor Gelin, DO
Lehigh Valley Health Network, Allentown, PA
Introduction: Each year 64,000 people in the United States are diagnosed with pancreatic cancer with 90% of the cases classified as exocrine tumors, commonly pancreatic adenocarcinoma. Less than 2% are diagnosed with pancreatic neuroendocrine tumor (PNET). Here we discuss a case of a patient with abdominal pain and watery diarrhea who was diagnosed with recurrent PNET and type 3c diabetes.
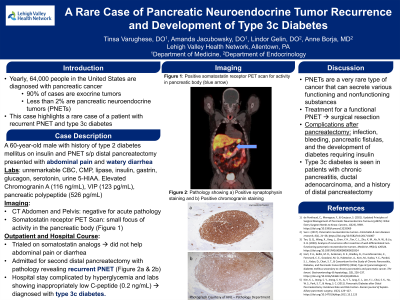
Case Description/Methods: A 60-year-old male with a history of type 2 diabetes mellitus on insulin and PNET status post distal pancreatectomy, presented to his physician with abdominal pain and watery diarrhea. His symptoms started 2 years after his surgery and worsened over 6 months. Basic laboratory testing including lipase was unremarkable. A CT of his abdomen was negative for acute pathology. With presentation similar to his previous diagnosis of PNET, specific laboratory testing showed elevated levels of Chromogranin A at 116 ng/mL, vasoactive intestinal peptide at 123 pg/mL, and pancreatic polypeptide at 526 pg/mL. Serum insulin, gastrin, glucagon, serotonin, and urine 5-HIAA levels were within normal range. A confirmatory somatostatin receptor PET scan revealed a small focus of activity in the pancreatic body. The patient was trialed on somatostatin analogs which did not control his symptoms. Ultimately, he underwent a second distal pancreatectomy with pathology revealing a recurrent PNET. His clinical course was complicated by hyperglycemia, undetectable insulin, and inappropriately low C-peptide of 0.2 ng/mL, leading to a diagnosis of type 3c diabetes.
Discussion: PNETs are a rare type of cancer that can secrete various functional hormones (insulin, gastrin, glucagon, and VIP) and nonfunctioning substances. Disease recurrence has been noted in 21-42% of all cases and more commonly occurs in those patients with underlying insulinomas, metastases, or locally advanced disease. A PNET is diagnosed by biopsy or imaging with radiolabeled somatostatin analogs. Treatment for a functional tumor includes resection to prevent malignant transformation and reduce hormone hypersecretion. Complications following pancreatectomy are infection, pancreatic fistulas, and the development of diabetes. Type 3c diabetes is seen in patients with chronic pancreatitis, ductal adenocarcinoma, and history of distal pancreatectomy. A 2011 study showed that 80% of patients with type 3c diabetes developed symptoms within a year of the surgery. This emphasizes the need to monitor glycemic control following pancreatectomy for recurrent PNET.
Disclosures:
Tinsa Varughese, DO, Amanda Jacubowsky, DO, Anne Borja, MD, Lindor Gelin, DO. P3550 - A Case of Pancreatic Neuroendocrine Tumor Recurrence and Development of Type 3c diabetes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Lehigh Valley Health Network, Allentown, PA
Introduction: Each year 64,000 people in the United States are diagnosed with pancreatic cancer with 90% of the cases classified as exocrine tumors, commonly pancreatic adenocarcinoma. Less than 2% are diagnosed with pancreatic neuroendocrine tumor (PNET). Here we discuss a case of a patient with abdominal pain and watery diarrhea who was diagnosed with recurrent PNET and type 3c diabetes.
Case Description/Methods: A 60-year-old male with a history of type 2 diabetes mellitus on insulin and PNET status post distal pancreatectomy, presented to his physician with abdominal pain and watery diarrhea. His symptoms started 2 years after his surgery and worsened over 6 months. Basic laboratory testing including lipase was unremarkable. A CT of his abdomen was negative for acute pathology. With presentation similar to his previous diagnosis of PNET, specific laboratory testing showed elevated levels of Chromogranin A at 116 ng/mL, vasoactive intestinal peptide at 123 pg/mL, and pancreatic polypeptide at 526 pg/mL. Serum insulin, gastrin, glucagon, serotonin, and urine 5-HIAA levels were within normal range. A confirmatory somatostatin receptor PET scan revealed a small focus of activity in the pancreatic body. The patient was trialed on somatostatin analogs which did not control his symptoms. Ultimately, he underwent a second distal pancreatectomy with pathology revealing a recurrent PNET. His clinical course was complicated by hyperglycemia, undetectable insulin, and inappropriately low C-peptide of 0.2 ng/mL, leading to a diagnosis of type 3c diabetes.
Discussion: PNETs are a rare type of cancer that can secrete various functional hormones (insulin, gastrin, glucagon, and VIP) and nonfunctioning substances. Disease recurrence has been noted in 21-42% of all cases and more commonly occurs in those patients with underlying insulinomas, metastases, or locally advanced disease. A PNET is diagnosed by biopsy or imaging with radiolabeled somatostatin analogs. Treatment for a functional tumor includes resection to prevent malignant transformation and reduce hormone hypersecretion. Complications following pancreatectomy are infection, pancreatic fistulas, and the development of diabetes. Type 3c diabetes is seen in patients with chronic pancreatitis, ductal adenocarcinoma, and history of distal pancreatectomy. A 2011 study showed that 80% of patients with type 3c diabetes developed symptoms within a year of the surgery. This emphasizes the need to monitor glycemic control following pancreatectomy for recurrent PNET.
Disclosures:
Tinsa Varughese indicated no relevant financial relationships.
Amanda Jacubowsky indicated no relevant financial relationships.
Anne Borja indicated no relevant financial relationships.
Lindor Gelin indicated no relevant financial relationships.
Tinsa Varughese, DO, Amanda Jacubowsky, DO, Anne Borja, MD, Lindor Gelin, DO. P3550 - A Case of Pancreatic Neuroendocrine Tumor Recurrence and Development of Type 3c diabetes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
