Tuesday Poster Session
Category: Biliary/Pancreas
P3572 - Pancreatic Metastasis From Papillary Thyroid Cancer as an Unusual Cause of Pancreatic Mass Lesion: A Case Report and Review of the Literature
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
Jodie A. Barkin, MD, FACG
University of Miami Miller School of Medicine
Boca Raton, FL
Presenting Author(s)
Sunny Sandhu, MD1, Julio Poveda, MD1, Jodie A. Barkin, MD, FACG2
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami Miller School of Medicine, Boca Raton, FL
Introduction: Papillary thyroid cancer (PTC), the most common endocrine malignancy, typically is a localized malignancy with an excellent long-term prognosis. Metastases most often occur locally to lymph nodes; however about 5% of patients have distant metastases occurring predominantly to bones and lungs. Pancreatic metastases from PTC are extremely rare, with only 19 cases described. Our aim is to report a case of metastatic PTC to the pancreas and review the literature.
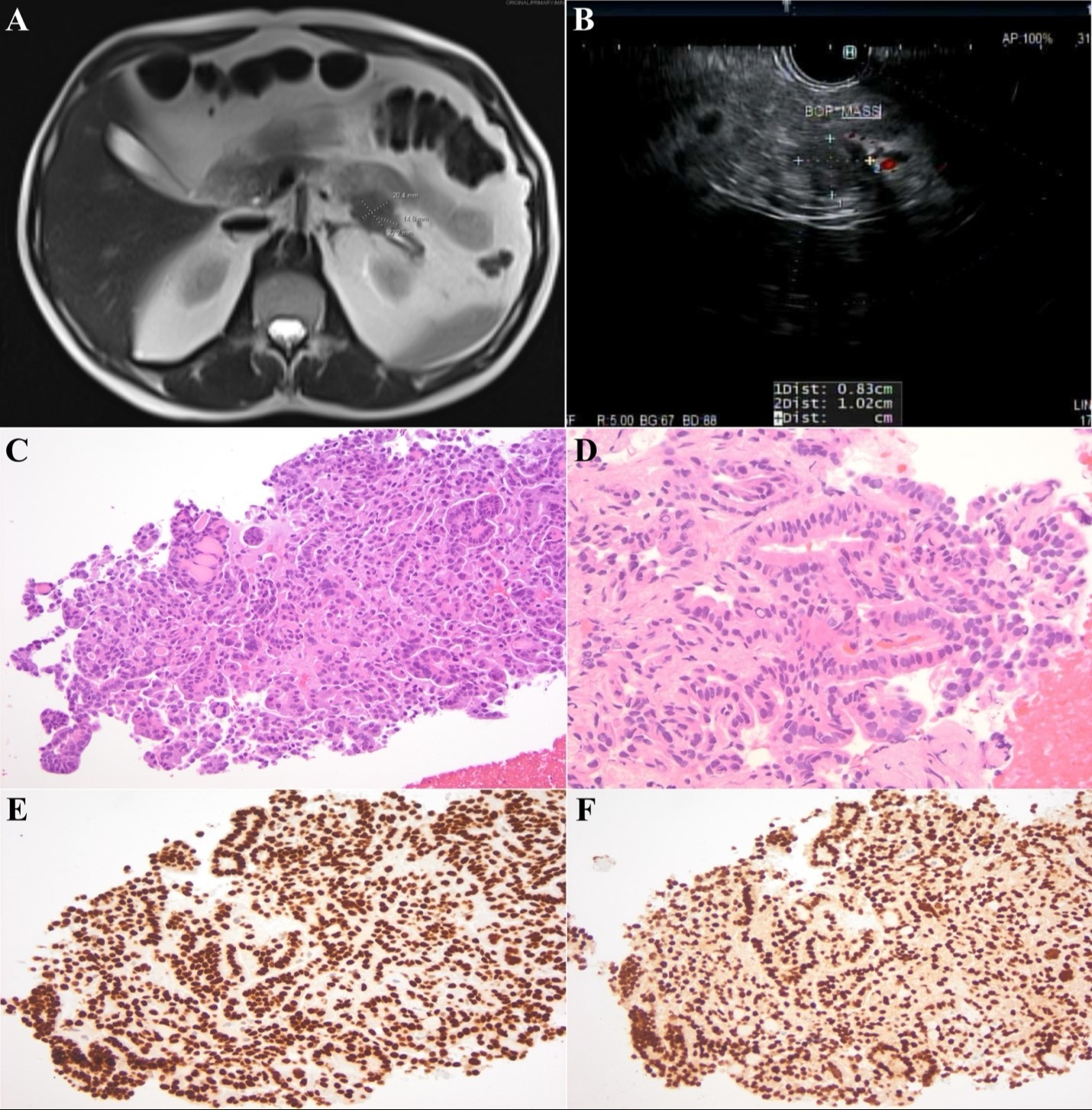
Case Description/Methods: A 56-year-old male with history of tall-cell PTC diagnosed 8 years prior, treated with thyroidectomy and radioactive iodine was referred for evaluation of a new pancreatic mass. 3 years prior, he was found to have PTC recurrence with a localized metastasis to C6 vertebra, successfully treated with radiation, and followed on active surveillance. Magnetic resonance imaging (MRI) showed a solid mass within the distal body/tail of the pancreas measuring 2 cm (Figure 1); CA 19-9 was < 3 U/mL. Endoscopic ultrasound (EUS) showed a hypoechoic round mass measuring 12.3 x 11.9mm with poorly defined borders, and upstream pancreatic atrophy and pancreatic duct dilation to 3.6mm (Figure 1). Fine needle biopsy (FNB) revealed cells positive for TTF-1, PAX8 and thyroglobulin, consistent with metastatic PTC (Figure 1). Given multiple sites of metastases, he was started on dabrafenib and trametinib and has done well during follow-up.
Discussion: Pancreatic metastases from PTC are extremely rare, with 12 studies of 19 cases from 2006-2023 described in the literature thus far. Most cases have been described in males (84%), with mean age of 62 years (standard deviation ± 12.9). Tall-cell PTC is more common than the follicular variant (21% vs. 11%). Diagnostic imaging may be non-specific, as metastatic PTC to the pancreas can appear similar to a primary pancreatic malignancy. EUS-guided FNB is diagnostic and should be performed to define histology and guide subsequent therapies especially in those with history of PTC. Treatment should target the underlying metastatic PTC, with systemic treatment and surgical resection described, with surgery shown to increase survival rates when performed for isolated pancreatic metastases in fit patients. Clinicians should be aware of PTC pancreatic metastases as a disease process given potential overlap of pathologic features of glandular epithelium with pancreatic adenocarcinoma and the markedly different treatment strategies and prognoses of these distinct entities.
Disclosures:
Sunny Sandhu, MD1, Julio Poveda, MD1, Jodie A. Barkin, MD, FACG2. P3572 - Pancreatic Metastasis From Papillary Thyroid Cancer as an Unusual Cause of Pancreatic Mass Lesion: A Case Report and Review of the Literature, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Miami Miller School of Medicine, Miami, FL; 2University of Miami Miller School of Medicine, Boca Raton, FL
Introduction: Papillary thyroid cancer (PTC), the most common endocrine malignancy, typically is a localized malignancy with an excellent long-term prognosis. Metastases most often occur locally to lymph nodes; however about 5% of patients have distant metastases occurring predominantly to bones and lungs. Pancreatic metastases from PTC are extremely rare, with only 19 cases described. Our aim is to report a case of metastatic PTC to the pancreas and review the literature.
Case Description/Methods: A 56-year-old male with history of tall-cell PTC diagnosed 8 years prior, treated with thyroidectomy and radioactive iodine was referred for evaluation of a new pancreatic mass. 3 years prior, he was found to have PTC recurrence with a localized metastasis to C6 vertebra, successfully treated with radiation, and followed on active surveillance. Magnetic resonance imaging (MRI) showed a solid mass within the distal body/tail of the pancreas measuring 2 cm (Figure 1); CA 19-9 was < 3 U/mL. Endoscopic ultrasound (EUS) showed a hypoechoic round mass measuring 12.3 x 11.9mm with poorly defined borders, and upstream pancreatic atrophy and pancreatic duct dilation to 3.6mm (Figure 1). Fine needle biopsy (FNB) revealed cells positive for TTF-1, PAX8 and thyroglobulin, consistent with metastatic PTC (Figure 1). Given multiple sites of metastases, he was started on dabrafenib and trametinib and has done well during follow-up.
Discussion: Pancreatic metastases from PTC are extremely rare, with 12 studies of 19 cases from 2006-2023 described in the literature thus far. Most cases have been described in males (84%), with mean age of 62 years (standard deviation ± 12.9). Tall-cell PTC is more common than the follicular variant (21% vs. 11%). Diagnostic imaging may be non-specific, as metastatic PTC to the pancreas can appear similar to a primary pancreatic malignancy. EUS-guided FNB is diagnostic and should be performed to define histology and guide subsequent therapies especially in those with history of PTC. Treatment should target the underlying metastatic PTC, with systemic treatment and surgical resection described, with surgery shown to increase survival rates when performed for isolated pancreatic metastases in fit patients. Clinicians should be aware of PTC pancreatic metastases as a disease process given potential overlap of pathologic features of glandular epithelium with pancreatic adenocarcinoma and the markedly different treatment strategies and prognoses of these distinct entities.
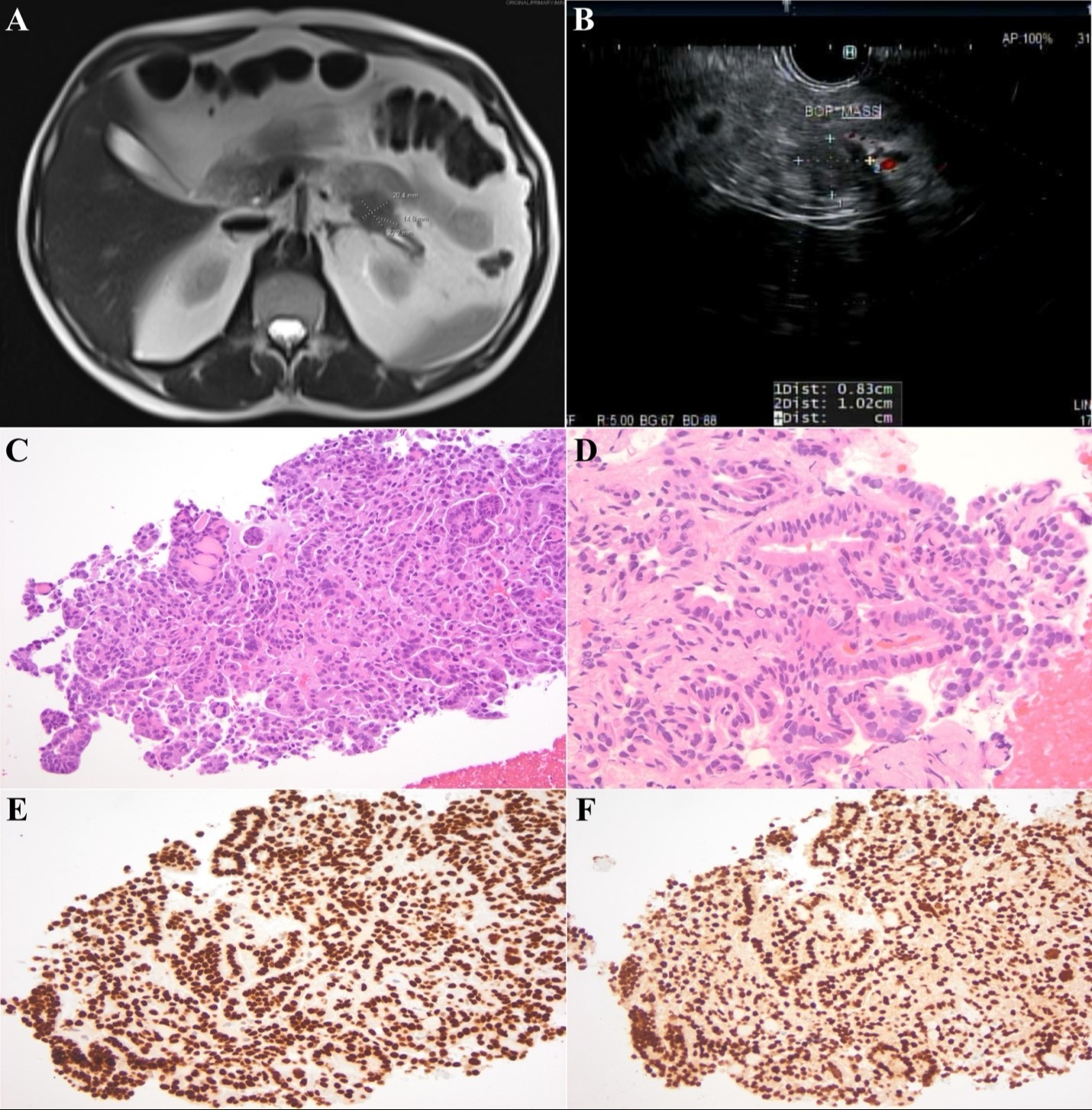
Figure: Figure 1: (A): Magnetic resonance imaging (MRI) showing a solid mass within the distal body/tail of the pancreas measuring 2 cm. (B): Endoscopic ultrasound (EUS) showing a hypoechoic round mass measuring 12.3 x 11.9mm with poorly defined borders. (C): Histologic sections consist of carcinoma that is present forming small microfollicles and small papillae. The neoplastic cells are small to intermediate in size with ground glass nuclei and abundant eosinophilic cytoplasm. Colloid formation is also readily seen. (D): The carcinoma is present forming small papillae. Numerous neoplastic cells demonstrate nuclear pseudoinclusions. (E): The carcinoma is diffusely positive for TTF-1 immunohistochemistry. (F): PAX-8 immunohistochemistry is also diffusely positive, supporting thyroid origin.
Disclosures:
Sunny Sandhu indicated no relevant financial relationships.
Julio Poveda indicated no relevant financial relationships.
Jodie Barkin: Abbvie – Consultant. Aimmune Therapeutics – Consultant. Corevitas – Consultant. Exact Sciences – Consultant. Medtronic – Consultant. Motus GI – Consultant. Organon – Consultant.
Sunny Sandhu, MD1, Julio Poveda, MD1, Jodie A. Barkin, MD, FACG2. P3572 - Pancreatic Metastasis From Papillary Thyroid Cancer as an Unusual Cause of Pancreatic Mass Lesion: A Case Report and Review of the Literature, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
