Tuesday Poster Session
Category: Biliary/Pancreas
P3610 - Rapidly Progressive Hypertriglyceridemia Induced Necrotizing Pancreatitis Refractory to High Dose Insulin Infusion
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JJ
Jason John, DO
Jefferson Health
Pennsauken, NJ
Presenting Author(s)
Jason John, DO1, Brian Blair, DO2, Lucy Joo, DO2, C. Jonathan Foster, DO2, Matthew Everwine, DO3, Edward Bley, DO3, Neethi Dasu, DO4
1Jefferson Health, Pennsauken, NJ; 2Jefferson Health, Cherry Hill, NJ; 3Jefferson Health, Washington Township, NJ; 4Beth Israel Lahey Health, Burlington, MA
Introduction: Hypertriglycedemia-induced pancreatitis (HTGP) is an infrequent cause of acute pancreatitis. It is typically seen when triglyceride levels exceed 1000 mg/dl, with clinical outcomes worsening with persistent elevations. The management of this condition targets triglyceride reduction, with insulin infusion usually being the first-line therapy. We present a unique case of a 47-year-old male with acute necrotizing pancreatitis refractory to high-dose insulin infusion requiring plasmapheresis.
Case Description/Methods: A 47-year-old male presented with a two-day history of epigastric abdominal pain. Initial lab work was notable for a lipase of 738 u/L and triglycerides of 2438 mg/dL. CT Abdomen/Pelvis without IV contrast showed findings compatible with peripancreatic fat strandiing with possible peripancreatic fluid collection. Six hours later, the patient’s abdominal pain and distension significantly worsened, prompting an emergent repeat CT scan, which showed severe necrotizing pancreatitis with a developing pseudocyst at the tail of the pancreas measuring 3.8 cm x 5.2 cm x 4.1 cm. Bladder pressures were also noted to be elevated at 20 ml/cm H2O, and he was transferred to the intensive care unit due to concern for abdominal compartment syndrome and new-onset renal failure. He was started on a high-dose insulin infusion; however, his triglycerides remained >1000 mg/dl. The decision was made to initiate total plasma exchange (TPE) for triglyceride clearance, which yielded a 50% reduction in serum triglyceride levels after only one session. His triglycerides were serially monitored and were noted to be as low as 238mg/dL within a few days. He was discharged home with maintenance Fenofibrate.
Discussion: In patients with severe HTG-AP, the goal of lowering serum triglycerides rapidly is of utmost importance in improving mortality. IV Insulin infusion is typically the first-line treatment for HTG-AP, given it is the more accessible and least expensive option. However, in our case, given there was no improvement with insulin, initiation of plasmapheresis was necessary. Therapeutic plasmapheresis has been suggested as a potential treatment approach for HTG-AP; however, it remains unclear if this offers an additional benefit compared to more conventional management. Our case proved that therapeutic plasmapheresis is an effective method in managing hypertriglyceridemia-induced necrotizing pancreatitis and mitigating potential complications such as abdominal compartment syndrome.

Disclosures:
Jason John, DO1, Brian Blair, DO2, Lucy Joo, DO2, C. Jonathan Foster, DO2, Matthew Everwine, DO3, Edward Bley, DO3, Neethi Dasu, DO4. P3610 - Rapidly Progressive Hypertriglyceridemia Induced Necrotizing Pancreatitis Refractory to High Dose Insulin Infusion, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jefferson Health, Pennsauken, NJ; 2Jefferson Health, Cherry Hill, NJ; 3Jefferson Health, Washington Township, NJ; 4Beth Israel Lahey Health, Burlington, MA
Introduction: Hypertriglycedemia-induced pancreatitis (HTGP) is an infrequent cause of acute pancreatitis. It is typically seen when triglyceride levels exceed 1000 mg/dl, with clinical outcomes worsening with persistent elevations. The management of this condition targets triglyceride reduction, with insulin infusion usually being the first-line therapy. We present a unique case of a 47-year-old male with acute necrotizing pancreatitis refractory to high-dose insulin infusion requiring plasmapheresis.
Case Description/Methods: A 47-year-old male presented with a two-day history of epigastric abdominal pain. Initial lab work was notable for a lipase of 738 u/L and triglycerides of 2438 mg/dL. CT Abdomen/Pelvis without IV contrast showed findings compatible with peripancreatic fat strandiing with possible peripancreatic fluid collection. Six hours later, the patient’s abdominal pain and distension significantly worsened, prompting an emergent repeat CT scan, which showed severe necrotizing pancreatitis with a developing pseudocyst at the tail of the pancreas measuring 3.8 cm x 5.2 cm x 4.1 cm. Bladder pressures were also noted to be elevated at 20 ml/cm H2O, and he was transferred to the intensive care unit due to concern for abdominal compartment syndrome and new-onset renal failure. He was started on a high-dose insulin infusion; however, his triglycerides remained >1000 mg/dl. The decision was made to initiate total plasma exchange (TPE) for triglyceride clearance, which yielded a 50% reduction in serum triglyceride levels after only one session. His triglycerides were serially monitored and were noted to be as low as 238mg/dL within a few days. He was discharged home with maintenance Fenofibrate.
Discussion: In patients with severe HTG-AP, the goal of lowering serum triglycerides rapidly is of utmost importance in improving mortality. IV Insulin infusion is typically the first-line treatment for HTG-AP, given it is the more accessible and least expensive option. However, in our case, given there was no improvement with insulin, initiation of plasmapheresis was necessary. Therapeutic plasmapheresis has been suggested as a potential treatment approach for HTG-AP; however, it remains unclear if this offers an additional benefit compared to more conventional management. Our case proved that therapeutic plasmapheresis is an effective method in managing hypertriglyceridemia-induced necrotizing pancreatitis and mitigating potential complications such as abdominal compartment syndrome.

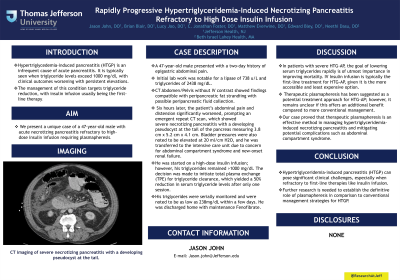
Figure: CT imaging of severe necrotizing pancreatitis with a developing pseudocyst at the tail.
Disclosures:
Jason John indicated no relevant financial relationships.
Brian Blair indicated no relevant financial relationships.
Lucy Joo indicated no relevant financial relationships.
C. Jonathan Foster: Conmed – Consultant. Steris – Consultant.
Matthew Everwine indicated no relevant financial relationships.
Edward Bley indicated no relevant financial relationships.
Neethi Dasu indicated no relevant financial relationships.
Jason John, DO1, Brian Blair, DO2, Lucy Joo, DO2, C. Jonathan Foster, DO2, Matthew Everwine, DO3, Edward Bley, DO3, Neethi Dasu, DO4. P3610 - Rapidly Progressive Hypertriglyceridemia Induced Necrotizing Pancreatitis Refractory to High Dose Insulin Infusion, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
