Tuesday Poster Session
Category: Biliary/Pancreas
P3616 - Hemosuccus Pancreaticus: A Hidden Gastrointestinal Challenge
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Muhammad F. Bouso, MD, MS
New York-Presbyterian Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Muhammad F. Bouso, MD, MS1, Harsh Patel, MD2, Anas Zaher, MD2, Nicholas Brown, MD1, Navim Mobin, MD1
1New York-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Hemosuccus pancreaticus (HP) is a rare cause of upper gastrointestinal (GI) bleeding. Originating from the pancreatic duct, HP accounts for about 1 in 1500 cases of upper GI hemorrhage and carries a risk of mortality up to 9.8%. Typically diagnosed via esophagogastroduodenscopy (EGD) or CT angiogram (CTA), HP can arise from pseudoaneurysms in peripancreatic vasculature, pancreatic tumors, pancreatitis-associated arterial erosion, or idiopathic causes. We present two conservatively managed cases of HP.
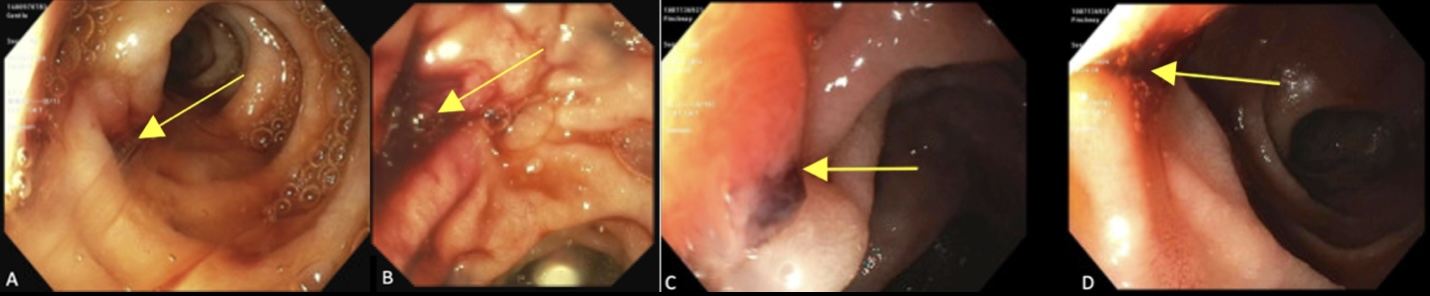
Case Description/Methods: Case 1:
A 70-year-old male with a past medical history (PMHx) of congestive heart failure, end-stage renal disease, and atrial fibrillation on Eliquis presented to the emergency department (ED) after multiple episodes of coffee ground emesis and melena. His hemoglobin (hgb) on admission was 9.8 g/dL with suboptimal response to transfusion, requiring 4 units of packet red blood cells (pRBC). He underwent EGD which visualized active bleeding from the ampulla of Vater (Figure 1A & 1B). Magnetic resonance cholangiopancreatography and abdominal MRI showed dilated biliary and pancreatic ducts with no active bleeding, mass, pancreatitis, or pseudoaneurysm. His bleeding was thus believed to be idiopathic, exacerbated by his home Eliquis. His melena resolved and hgb stabilized without further intervention. However, he was lost to follow-up after discharge.
Case 2:
A 67-year-old male with a PMHx of alcohol use disorder complicated by chronic pancreatitis and decompensated liver cirrhosis presented to the ED due to epigastric pain. He was found to have acute alcoholic hepatitis and acute on chronic pancreatitis. He later developed melanic stool with a 3 g/dL decline in his hgb. He underwent EGD which visualized bleeding from the ampulla of Vater (Figure 1C & 1D). A CTA showed pancreatic calcifications and ductal dilatation and no active bleeding or pseudoaneurysms. He was managed with pRBC transfusion and his hgb stabilized without further intervention. He is well 2 months after discharge without recurrent bleeding.
Discussion: HP is a rare condition that can manifest with abdominal pain, GI bleeding, and hemodynamic instability. Traditional management involves fluid resuscitation, blood transfusion, and arterial embolization. However, our cases demonstrate clinical scenarios where HP can occasionally be managed conservatively. Further research into the causes, diagnosis, and protocols for HP is needed to enhance our understanding and improve care for this challenging condition.
Disclosures:
Muhammad F. Bouso, MD, MS1, Harsh Patel, MD2, Anas Zaher, MD2, Nicholas Brown, MD1, Navim Mobin, MD1. P3616 - Hemosuccus Pancreaticus: A Hidden Gastrointestinal Challenge, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2New York-Presbyterian / Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Hemosuccus pancreaticus (HP) is a rare cause of upper gastrointestinal (GI) bleeding. Originating from the pancreatic duct, HP accounts for about 1 in 1500 cases of upper GI hemorrhage and carries a risk of mortality up to 9.8%. Typically diagnosed via esophagogastroduodenscopy (EGD) or CT angiogram (CTA), HP can arise from pseudoaneurysms in peripancreatic vasculature, pancreatic tumors, pancreatitis-associated arterial erosion, or idiopathic causes. We present two conservatively managed cases of HP.
Case Description/Methods: Case 1:
A 70-year-old male with a past medical history (PMHx) of congestive heart failure, end-stage renal disease, and atrial fibrillation on Eliquis presented to the emergency department (ED) after multiple episodes of coffee ground emesis and melena. His hemoglobin (hgb) on admission was 9.8 g/dL with suboptimal response to transfusion, requiring 4 units of packet red blood cells (pRBC). He underwent EGD which visualized active bleeding from the ampulla of Vater (Figure 1A & 1B). Magnetic resonance cholangiopancreatography and abdominal MRI showed dilated biliary and pancreatic ducts with no active bleeding, mass, pancreatitis, or pseudoaneurysm. His bleeding was thus believed to be idiopathic, exacerbated by his home Eliquis. His melena resolved and hgb stabilized without further intervention. However, he was lost to follow-up after discharge.
Case 2:
A 67-year-old male with a PMHx of alcohol use disorder complicated by chronic pancreatitis and decompensated liver cirrhosis presented to the ED due to epigastric pain. He was found to have acute alcoholic hepatitis and acute on chronic pancreatitis. He later developed melanic stool with a 3 g/dL decline in his hgb. He underwent EGD which visualized bleeding from the ampulla of Vater (Figure 1C & 1D). A CTA showed pancreatic calcifications and ductal dilatation and no active bleeding or pseudoaneurysms. He was managed with pRBC transfusion and his hgb stabilized without further intervention. He is well 2 months after discharge without recurrent bleeding.
Discussion: HP is a rare condition that can manifest with abdominal pain, GI bleeding, and hemodynamic instability. Traditional management involves fluid resuscitation, blood transfusion, and arterial embolization. However, our cases demonstrate clinical scenarios where HP can occasionally be managed conservatively. Further research into the causes, diagnosis, and protocols for HP is needed to enhance our understanding and improve care for this challenging condition.
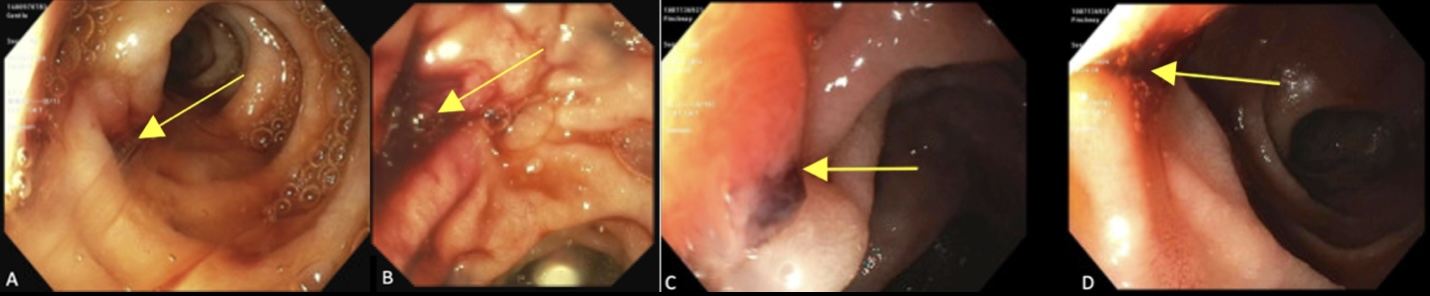
Figure: Figures 1A & 1B: Fresh blood mixed with bile at the ampulla of Vater from Case 1
Figures 1C & 1D: Active bleeding arising from the ampulla of Vater from Case 2
Figures 1C & 1D: Active bleeding arising from the ampulla of Vater from Case 2
Disclosures:
Muhammad Bouso indicated no relevant financial relationships.
Harsh Patel indicated no relevant financial relationships.
Anas Zaher indicated no relevant financial relationships.
Nicholas Brown indicated no relevant financial relationships.
Navim Mobin indicated no relevant financial relationships.
Muhammad F. Bouso, MD, MS1, Harsh Patel, MD2, Anas Zaher, MD2, Nicholas Brown, MD1, Navim Mobin, MD1. P3616 - Hemosuccus Pancreaticus: A Hidden Gastrointestinal Challenge, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
