Tuesday Poster Session
Category: Colon
P3629 - Prevalence and Clinical Characteristics of Serrated Adenomas at Screening Colonoscopy in Rural Georgians
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SB
Sheena Bhushan, MD
Northeast Georgia Medical Center
Buford, GA
Presenting Author(s)
Sheena Bhushan, MD1, Abijha Boban, DO, MBA2, Adeoluwa Adewuyi, MD2, Shane Robinson, MS3, Ania Rynarzewska, PhD2, Idopise Umana, MD2, Kenneth Vega, MD, FACG4
1Northeast Georgia Medical Center, Buford, GA; 2Northeast Georgia Medical Center, Atlanta, GA; 3Northeast Georgia Medical Center, Gainesville, GA; 4Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Serrated adenomas are a precursor lesion for colorectal cancer (CRC) and account for ~15-30% of all colorectal polyps, thus making their detection and characterization crucial. There is currently minimal data evaluating serrated adenoma prevalence in community and rural settings. This study aims to investigate the prevalence, clinical characteristics, and racial/ethnic variability of serrated adenomas among patients undergoing screening colonoscopy in a community hospital system in rural Georgia.
Methods: A retrospective cross-sectional chart review was performed of patients who underwent screening colonoscopy (SC) within a community health system from 2016-2024. Patients with histologically proven serrated adenomas found at SC were included. Data on polyp size, location (right, transverse, left colon and/or rectal), patient race/ethnicity, insurance type, BMI and habits (alcohol consumption and smoking status) were collected. Data were analyzed using frequencies, Chi square tests and logistic regression models.
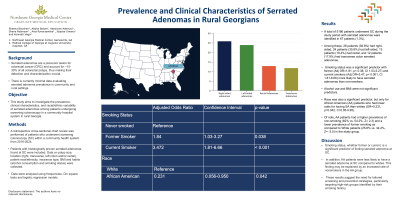
Results: A total of 5186 patients underwent SC during the study period with serrated adenomas were identified in 67 patients (1.3%). Among these, 26 patients (38.8%) had right-sided, 24 patients (35.8%) had left-sided, 13 patients (19.4%) had rectal, and 12 patients (17.9%) had transverse colon serrated adenomas. Smoking status was a significant predictor with former (Adj OR=1.81, p< 0.38, CI 1.03-3.27) and current smokers (Adj OR=3.47, p< 0.001, CI 1.81-6.66) more likely to have serrated adenomas than non-smokers. Alcohol use and BMI were not significant predictors. Race was also a significant predictor, but only for African American (AA) patients who had lower odds for having SA than whites (OR=0.231, p=0.042, CI 0.05-0.95). Of note, AA patients had a higher prevalence of non-smoking (62% vs. 54.2%, Z= 2.3) and a lower prevalence of former smoking as compared to White patients (25.8% vs. 34.2%, Z= -3.0) in the study group.
Discussion: Smoking status, whether former or current, is a significant predictor of finding serrated adenoma at SC. In addition, AA patients were less likely to have a serrated adenoma at SC compared to whites. This finding may be explained by an increased rate of nonsmokers in the AA group. These results suggest the need for tailored screening and prevention strategies, particularly targeting high-risk groups identified by their smoking history.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheena Bhushan, MD1, Abijha Boban, DO, MBA2, Adeoluwa Adewuyi, MD2, Shane Robinson, MS3, Ania Rynarzewska, PhD2, Idopise Umana, MD2, Kenneth Vega, MD, FACG4. P3629 - Prevalence and Clinical Characteristics of Serrated Adenomas at Screening Colonoscopy in Rural Georgians, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Northeast Georgia Medical Center, Buford, GA; 2Northeast Georgia Medical Center, Atlanta, GA; 3Northeast Georgia Medical Center, Gainesville, GA; 4Medical College of Georgia at Augusta University, Augusta, GA
Introduction: Serrated adenomas are a precursor lesion for colorectal cancer (CRC) and account for ~15-30% of all colorectal polyps, thus making their detection and characterization crucial. There is currently minimal data evaluating serrated adenoma prevalence in community and rural settings. This study aims to investigate the prevalence, clinical characteristics, and racial/ethnic variability of serrated adenomas among patients undergoing screening colonoscopy in a community hospital system in rural Georgia.
Methods: A retrospective cross-sectional chart review was performed of patients who underwent screening colonoscopy (SC) within a community health system from 2016-2024. Patients with histologically proven serrated adenomas found at SC were included. Data on polyp size, location (right, transverse, left colon and/or rectal), patient race/ethnicity, insurance type, BMI and habits (alcohol consumption and smoking status) were collected. Data were analyzed using frequencies, Chi square tests and logistic regression models.
Results: A total of 5186 patients underwent SC during the study period with serrated adenomas were identified in 67 patients (1.3%). Among these, 26 patients (38.8%) had right-sided, 24 patients (35.8%) had left-sided, 13 patients (19.4%) had rectal, and 12 patients (17.9%) had transverse colon serrated adenomas. Smoking status was a significant predictor with former (Adj OR=1.81, p< 0.38, CI 1.03-3.27) and current smokers (Adj OR=3.47, p< 0.001, CI 1.81-6.66) more likely to have serrated adenomas than non-smokers. Alcohol use and BMI were not significant predictors. Race was also a significant predictor, but only for African American (AA) patients who had lower odds for having SA than whites (OR=0.231, p=0.042, CI 0.05-0.95). Of note, AA patients had a higher prevalence of non-smoking (62% vs. 54.2%, Z= 2.3) and a lower prevalence of former smoking as compared to White patients (25.8% vs. 34.2%, Z= -3.0) in the study group.
Discussion: Smoking status, whether former or current, is a significant predictor of finding serrated adenoma at SC. In addition, AA patients were less likely to have a serrated adenoma at SC compared to whites. This finding may be explained by an increased rate of nonsmokers in the AA group. These results suggest the need for tailored screening and prevention strategies, particularly targeting high-risk groups identified by their smoking history.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheena Bhushan indicated no relevant financial relationships.
Abijha Boban indicated no relevant financial relationships.
Adeoluwa Adewuyi indicated no relevant financial relationships.
Shane Robinson indicated no relevant financial relationships.
Ania Rynarzewska indicated no relevant financial relationships.
Idopise Umana indicated no relevant financial relationships.
Kenneth Vega indicated no relevant financial relationships.
Sheena Bhushan, MD1, Abijha Boban, DO, MBA2, Adeoluwa Adewuyi, MD2, Shane Robinson, MS3, Ania Rynarzewska, PhD2, Idopise Umana, MD2, Kenneth Vega, MD, FACG4. P3629 - Prevalence and Clinical Characteristics of Serrated Adenomas at Screening Colonoscopy in Rural Georgians, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
