Tuesday Poster Session
Category: Colon
P3631 - Systematic Literature Review and Meta-Analysis of Live Fecal Microbiota Therapeutics for Recurrent Clostridioides Difficile Infection
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CM
Conor McCloskey, PhD
Clarivate
London, England, United Kingdom
Presenting Author(s)
Conor McCloskey, PhD1, Corinne Le Reun, MSc2, Dianne Nguyen, MD, MBA3, Carl V. Crawford, MD4, Darrell S. Pardi, MD, MS5, Sunita Nair, PhD6, Jane De Vries, MSc7, Mark Wilcox, MD8
1Clarivate, London, England, United Kingdom; 2Independent, Guadeloupe, Guadeloupe, France; 3Nestlé Health Science, Bridgewater, NJ; 4New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 5Mayo Clinic, Rochester, MN; 6CLARIVATE, London, England, United Kingdom; 7Independent Health Economist, Bagshot, England, United Kingdom; 8University of Leeds, Leeds, England, United Kingdom
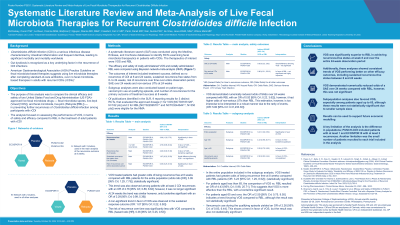
Introduction: Clostridioides difficile infection (CDI) is a debilitating, potentially fatal infectious disease of the gastrointestinal tract. CDI treatment includes antibiotics which can further disrupt the gut microbiota and increase the risk of recurrence. AGA Practice Guideline on fecal microbiota-based therapies suggests use of live microbiota therapies upon completion of standard of care antibiotics over no fecal microbiota-based therapies in adults with recurrent CDIs (rCDIs). This study aimed to compare the clinical efficacy and safety of US FDA-approved live fecal microbiota therapeutics in preventing further disease recurrences among participants with 1 or more previous rCDI.
Methods: A systematic literature search (SLR) was conducted using the Medline, Embase and Cochrane databases to identify randomized, controlled trials (RCT) examining fecal microbiota therapeutics of interest in patients with rCDIs [fecal microbiota spores, live-brpk (VOS); fecal microbiota live-jslm (RBL)]. The efficacy and safety of oral VOS and rectally administered RBL were compared using Bayesian network-meta-analysis (NMA). Outcomes of interest included treatment success (defined as no recurrence of CDI) at 8 weeks, time to CDI recurrence (over 24 wks after receipt of microbiome therapy) and serious adverse events (SAE) over 24 weeks. Subgroup analyses by patient (pt) age were also conducted for the primary outcome of treatment success at 8 weeks.
Results: Of publications identified in the SLR, 9 reporting results for 3 distinct RCTs (1 for VOS [NCT03183128, N=182 pts] and 2 for RBL [NCT02299570 and NCT03244644, N=350 pts]) were eligible for the NMA. VOS treated pts had greater odds of being recurrence free at 8 weeks compared with RBL pts for the entire population (odds ratio, 3.09 [95% CrI; 1.29, 7.75]; statistically significant), those aged < 65 years (odds ratio, 4.43 [95% Crl; 0.98, 25.71]), and those aged ≥65 years (odds ratio, 2.59 [95% Crl; 0.75, 9.55]). The risk of recurrence over time was significantly less with VOS compared to RBL (hazard ratio, 0.36 [95% CrI; 0.25, 0.53]). VOS demonstrated numerically reduced odds of a SAE over 24 weeks compared with RBL.
Discussion: In an indirect comparison of treatment effectiveness of novel FDA-approved, fecal microbiota therapeutics among study participants with rCDIs, VOS resulted in significantly greater odds of being recurrence free at 8 weeks and had a reduced chance of a serious adverse event over 24 weeks, compared with RBL.
Disclosures:
Conor McCloskey, PhD1, Corinne Le Reun, MSc2, Dianne Nguyen, MD, MBA3, Carl V. Crawford, MD4, Darrell S. Pardi, MD, MS5, Sunita Nair, PhD6, Jane De Vries, MSc7, Mark Wilcox, MD8. P3631 - Systematic Literature Review and Meta-Analysis of Live Fecal Microbiota Therapeutics for Recurrent <i>Clostridioides Difficile</i> Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Clarivate, London, England, United Kingdom; 2Independent, Guadeloupe, Guadeloupe, France; 3Nestlé Health Science, Bridgewater, NJ; 4New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 5Mayo Clinic, Rochester, MN; 6CLARIVATE, London, England, United Kingdom; 7Independent Health Economist, Bagshot, England, United Kingdom; 8University of Leeds, Leeds, England, United Kingdom
Introduction: Clostridioides difficile infection (CDI) is a debilitating, potentially fatal infectious disease of the gastrointestinal tract. CDI treatment includes antibiotics which can further disrupt the gut microbiota and increase the risk of recurrence. AGA Practice Guideline on fecal microbiota-based therapies suggests use of live microbiota therapies upon completion of standard of care antibiotics over no fecal microbiota-based therapies in adults with recurrent CDIs (rCDIs). This study aimed to compare the clinical efficacy and safety of US FDA-approved live fecal microbiota therapeutics in preventing further disease recurrences among participants with 1 or more previous rCDI.
Methods: A systematic literature search (SLR) was conducted using the Medline, Embase and Cochrane databases to identify randomized, controlled trials (RCT) examining fecal microbiota therapeutics of interest in patients with rCDIs [fecal microbiota spores, live-brpk (VOS); fecal microbiota live-jslm (RBL)]. The efficacy and safety of oral VOS and rectally administered RBL were compared using Bayesian network-meta-analysis (NMA). Outcomes of interest included treatment success (defined as no recurrence of CDI) at 8 weeks, time to CDI recurrence (over 24 wks after receipt of microbiome therapy) and serious adverse events (SAE) over 24 weeks. Subgroup analyses by patient (pt) age were also conducted for the primary outcome of treatment success at 8 weeks.
Results: Of publications identified in the SLR, 9 reporting results for 3 distinct RCTs (1 for VOS [NCT03183128, N=182 pts] and 2 for RBL [NCT02299570 and NCT03244644, N=350 pts]) were eligible for the NMA. VOS treated pts had greater odds of being recurrence free at 8 weeks compared with RBL pts for the entire population (odds ratio, 3.09 [95% CrI; 1.29, 7.75]; statistically significant), those aged < 65 years (odds ratio, 4.43 [95% Crl; 0.98, 25.71]), and those aged ≥65 years (odds ratio, 2.59 [95% Crl; 0.75, 9.55]). The risk of recurrence over time was significantly less with VOS compared to RBL (hazard ratio, 0.36 [95% CrI; 0.25, 0.53]). VOS demonstrated numerically reduced odds of a SAE over 24 weeks compared with RBL.
Discussion: In an indirect comparison of treatment effectiveness of novel FDA-approved, fecal microbiota therapeutics among study participants with rCDIs, VOS resulted in significantly greater odds of being recurrence free at 8 weeks and had a reduced chance of a serious adverse event over 24 weeks, compared with RBL.
Disclosures:
Conor McCloskey indicated no relevant financial relationships.
Corinne Le Reun indicated no relevant financial relationships.
Dianne Nguyen: Abbvie – Stock-publicly held company(excluding mutual/index funds). bristol meyers squibb – Stock-publicly held company(excluding mutual/index funds). Nestle Health Science – Employee, Stock-publicly held company(excluding mutual/index funds).
Carl Crawford: Ferring – Grant/Research Support. Nestle – Speakers Bureau. Phathom – Speakers Bureau. Seres – Speakers Bureau. Vedanta – Grant/Research Support.
Darrell Pardi: AbbVie – Consultant. Applied molecular transport – Grant/Research Support. Finch – Grant/Research Support. Immunic – Consultant. Otsuka – Consultant. Pfizer – Grant/Research Support. Phantom Pharmaceuticals – Consultant. Seres – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Vedanta – Consultant, Grant/Research Support.
Sunita Nair indicated no relevant financial relationships.
Jane De Vries: Nestle Health Science – Independent Contractor.
Mark Wilcox: Seres – Advisor or Review Panel Member, Consultant, Grant/Research Support. Tillotts – Advisor or Review Panel Member, Consultant.
Conor McCloskey, PhD1, Corinne Le Reun, MSc2, Dianne Nguyen, MD, MBA3, Carl V. Crawford, MD4, Darrell S. Pardi, MD, MS5, Sunita Nair, PhD6, Jane De Vries, MSc7, Mark Wilcox, MD8. P3631 - Systematic Literature Review and Meta-Analysis of Live Fecal Microbiota Therapeutics for Recurrent <i>Clostridioides Difficile</i> Infection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
