Tuesday Poster Session
Category: Colon
P3647 - Audit on Rectal Adenocarcinoma Management: Missed Opportunity for Endoscopic Resection
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jenson Phung, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Jenson Phung, MD1, Suchapa Arayakarnkul, MD1, Rahul Karna, MD1, Natalie Wilson, MD1, Tessa Herman, MD2, Brian Hanson, MD3, Juan C. Manivel, MD3, Mohammad Bilal, MD2
1University of Minnesota, Minneapolis, MN; 2University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 3Minneapolis VA Health Care System, Minneapolis, MN
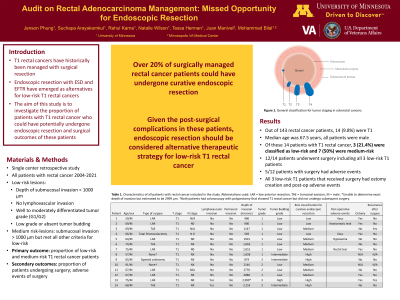
Introduction: Patients with T1 rectal cancer (RC) have historically received surgical resection. Endoscopic resection (ER) with endoscopic submucosal dissection (ESD) and endoscopic full-thickness resection (EFTR) has also emerged as a treatment option for low-risk T1 RC. We aimed to investigate the proportion and surgical outcomes of patients who could have potentially undergone ER for T1 RC.
Methods: A retrospective chart review was conducted for all patients with RC between 2004 and 2021 at our academic medical center prior to offering of ESD and EFTR at our institution. Demographic, clinical, oncologic, and surgical outcomes were reviewed for patients with T1 RC. A retrospective evaluation of pathology slides was performed by an experienced pathologist to assess prognostic histological features. Lesions were classified as low risk if they met all the following criteria: depth of submucosal invasion (SMI) < 1000 μm, no lymphovascular invasion, well-moderately differentiated (G1/G2) tumor grade, and low grade or absent tumor budding. These lesions would be considered to have undergone curative resection with ESD and EFTR if R0 resection is achieved. Lesions were classified as medium risk if depth of SMI > 1000 μm but met all other criteria for low risk lesions. Primary outcome was proportion of low risk and medium risk T1 RC patients. Secondary outcomes were proportion of patients undergoing surgery and associated adverse events (AEs).
Results: Out of 143 RC patients, 14 (9.8%) with T1 disease were included. Median age was 67.5 years, and all patients were male. Pathology review revealed 3 (21.4%) low-risk and 7 (50%) medium-risk T1 lesions. 12 / 14 patients (85.7%) underwent surgery including all 3 low risk RCs. Post-operative AEs occurred in 5 of the 12 patients (41.7%) who had surgery. All 3 patients with low risk T1 RC had an ostomy creation and had post-operative AEs. 2 patients (16.7%) had recurrence of their RC after surgery. Table 1 shows histological features and surgical outcomes of T1 RC patients.
Discussion: Our analysis suggests that over one-fifth of all surgically managed RC patients could potentially have undergone curative ER. All these patients had post-surgical AEs and ostomy creation. Endoscopic resection for low risk T1 RC can potentially have significant positive impact on morbidity and quality of life outcomes. Future larger prospective studies are needed to validate our findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jenson Phung, MD1, Suchapa Arayakarnkul, MD1, Rahul Karna, MD1, Natalie Wilson, MD1, Tessa Herman, MD2, Brian Hanson, MD3, Juan C. Manivel, MD3, Mohammad Bilal, MD2. P3647 - Audit on Rectal Adenocarcinoma Management: Missed Opportunity for Endoscopic Resection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 3Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Patients with T1 rectal cancer (RC) have historically received surgical resection. Endoscopic resection (ER) with endoscopic submucosal dissection (ESD) and endoscopic full-thickness resection (EFTR) has also emerged as a treatment option for low-risk T1 RC. We aimed to investigate the proportion and surgical outcomes of patients who could have potentially undergone ER for T1 RC.
Methods: A retrospective chart review was conducted for all patients with RC between 2004 and 2021 at our academic medical center prior to offering of ESD and EFTR at our institution. Demographic, clinical, oncologic, and surgical outcomes were reviewed for patients with T1 RC. A retrospective evaluation of pathology slides was performed by an experienced pathologist to assess prognostic histological features. Lesions were classified as low risk if they met all the following criteria: depth of submucosal invasion (SMI) < 1000 μm, no lymphovascular invasion, well-moderately differentiated (G1/G2) tumor grade, and low grade or absent tumor budding. These lesions would be considered to have undergone curative resection with ESD and EFTR if R0 resection is achieved. Lesions were classified as medium risk if depth of SMI > 1000 μm but met all other criteria for low risk lesions. Primary outcome was proportion of low risk and medium risk T1 RC patients. Secondary outcomes were proportion of patients undergoing surgery and associated adverse events (AEs).
Results: Out of 143 RC patients, 14 (9.8%) with T1 disease were included. Median age was 67.5 years, and all patients were male. Pathology review revealed 3 (21.4%) low-risk and 7 (50%) medium-risk T1 lesions. 12 / 14 patients (85.7%) underwent surgery including all 3 low risk RCs. Post-operative AEs occurred in 5 of the 12 patients (41.7%) who had surgery. All 3 patients with low risk T1 RC had an ostomy creation and had post-operative AEs. 2 patients (16.7%) had recurrence of their RC after surgery. Table 1 shows histological features and surgical outcomes of T1 RC patients.
Discussion: Our analysis suggests that over one-fifth of all surgically managed RC patients could potentially have undergone curative ER. All these patients had post-surgical AEs and ostomy creation. Endoscopic resection for low risk T1 RC can potentially have significant positive impact on morbidity and quality of life outcomes. Future larger prospective studies are needed to validate our findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jenson Phung indicated no relevant financial relationships.
Suchapa Arayakarnkul indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Natalie Wilson indicated no relevant financial relationships.
Tessa Herman indicated no relevant financial relationships.
Brian Hanson: Motus GI – Consultant.
Juan Manivel indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Jenson Phung, MD1, Suchapa Arayakarnkul, MD1, Rahul Karna, MD1, Natalie Wilson, MD1, Tessa Herman, MD2, Brian Hanson, MD3, Juan C. Manivel, MD3, Mohammad Bilal, MD2. P3647 - Audit on Rectal Adenocarcinoma Management: Missed Opportunity for Endoscopic Resection, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
