Tuesday Poster Session
Category: Colon
P3649 - Prevalence and Detection Rates of Serrated Polyps and Sessile Serrated Lesions in Average Risk Persons With Positive Fecal Immunohistochemical Test Undergoing Colonoscopy: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- FJ
Fouad Jaber, MD, MS
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Fouad Jaber, MD, MS1, Mohammad Jaber, MD2, Saqr Alsakarneh, MD1, Tala Alsharaeh, MD3, Abdelrahman Mohamed Mahmoud, MD4, Anas Alselek, MD5, Yazan Abboud, MD6, Mouhand F.H. Mohamed, MD7, Abubaker O. Abdalla, MD8, Khalid Ahmed, MD9, Mohamed Abdallah, MD10, Mohammad Bilal, MD11, Aasma Shaukat, MD, MPH12
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Al-Azhar University, Gaza, Palestinian Territories; 3The University of Jordan, Amman, 'Amman, Jordan; 4Menoufia University, Menoufia, Ad Daqahliyah, Egypt; 5Cairo University School of Medicine, Cairo, Al Jizah, Egypt; 6Rutgers New Jersey Medical School, Newark, NJ; 7Brown University, Providence, RI; 8Emory University, Atlanta, GA; 9University of Pennsylvania, Philadelphia, PA; 10Cleveland Clinic, Cleveland, OH; 11University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 12NYU Langone Health, New York, NY
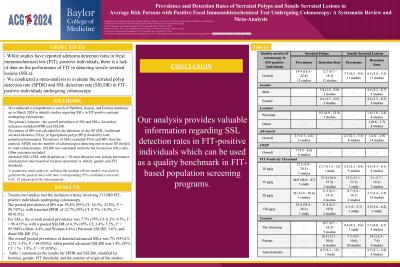
Introduction: While studies have reported adenoma detection rates in fecal immunochemical test (FIT) -positive individuals, there is a lack of data on the performance of FIT in detecting sessile serrated lesions (SSLs). Therefore, we conducted a meta-analysis to evaluate the serrated polyp detection rate (SPDR) and SSL detection rate (SSLDR) in FIT-positive individuals undergoing colonoscopy.
Methods: We conducted a comprehensive search of PubMed, Scopus, and Embase databases up to March 2024 to identify studies reporting SSLs in FIT-positive patients undergoing colonoscopy. The primary outcome was the overall prevalence of SPs and SSLs. Secondary outcomes included SPDR and SSLDR. Prevalence of SPs was calculated as the detection of any SP [SSL, traditional serrated adenoma (TSA), or hyperplastic polyp (HP)] divided by total patients/colonoscopies. Prevalence of SSLs excluded TSAs and HPs from the analysis. SPDR was the number of colonoscopies detecting one or more SP divided by total colonoscopies. SSLDR was calculated similarly but focused on SSLs only. Other outcomes included
advanced SSLs (SSL with dysplasia or ≥ 10 mm) detection rate, polyps prevenance and detection rates based on location (proximal vs. distal), gender, and FIT threshold. A proportion meta-analysis, utilizing the random effects model, was used to generate the pooled rates with their corresponding 95% confidence intervals (CI). I2 adjudicated the heterogeneity.
Results: Twenty-two studies met the inclusion criteria, involving 513,080 FIT-positive individuals undergoing colonoscopy. The pooled prevalence of SPs was 19.4% (95% CI: 16.5%–22.8%, I² = 99.747%), with a pooled SPDR of 12.7% (95% CI: 8.7%–18.3%, I² = 99.913%) (Men: 3.8%, and women: 4.2%). For SSLs, the overall pooled prevalence was 7.7% (95% CI: 6.2%–9.5%, I² = 99.415%), with a pooled SSLDR of 4.3% (95% CI: 3.4%–5.5%, I² = 99.586%) (Men: 4.4% and Women 4.4%) (Proximal SSLDR: 1.6%, and distal SSLDR 1%). The overall pooled prevalence of detected advanced SSLs was 7% (95%CI: 2.1%–3.5%, I² = 94.076%), while pooled advanced SSLDR was 1.4% (95% CI: 1 %– 1.9%, I² = 97.024%). Table 1 summarizes the results for SPDR and SSLDR, stratified by location, gender, FIT threshold, and the country of origin of the studies.
Discussion: Our analysis provides valuable information regarding SSL detection rates in FIT-positive individuals which can be used as a quality benchmark in FIT-based population screening programs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Fouad Jaber, MD, MS1, Mohammad Jaber, MD2, Saqr Alsakarneh, MD1, Tala Alsharaeh, MD3, Abdelrahman Mohamed Mahmoud, MD4, Anas Alselek, MD5, Yazan Abboud, MD6, Mouhand F.H. Mohamed, MD7, Abubaker O. Abdalla, MD8, Khalid Ahmed, MD9, Mohamed Abdallah, MD10, Mohammad Bilal, MD11, Aasma Shaukat, MD, MPH12. P3649 - Prevalence and Detection Rates of Serrated Polyps and Sessile Serrated Lesions in Average Risk Persons With Positive Fecal Immunohistochemical Test Undergoing Colonoscopy: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Al-Azhar University, Gaza, Palestinian Territories; 3The University of Jordan, Amman, 'Amman, Jordan; 4Menoufia University, Menoufia, Ad Daqahliyah, Egypt; 5Cairo University School of Medicine, Cairo, Al Jizah, Egypt; 6Rutgers New Jersey Medical School, Newark, NJ; 7Brown University, Providence, RI; 8Emory University, Atlanta, GA; 9University of Pennsylvania, Philadelphia, PA; 10Cleveland Clinic, Cleveland, OH; 11University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN; 12NYU Langone Health, New York, NY
Introduction: While studies have reported adenoma detection rates in fecal immunochemical test (FIT) -positive individuals, there is a lack of data on the performance of FIT in detecting sessile serrated lesions (SSLs). Therefore, we conducted a meta-analysis to evaluate the serrated polyp detection rate (SPDR) and SSL detection rate (SSLDR) in FIT-positive individuals undergoing colonoscopy.
Methods: We conducted a comprehensive search of PubMed, Scopus, and Embase databases up to March 2024 to identify studies reporting SSLs in FIT-positive patients undergoing colonoscopy. The primary outcome was the overall prevalence of SPs and SSLs. Secondary outcomes included SPDR and SSLDR. Prevalence of SPs was calculated as the detection of any SP [SSL, traditional serrated adenoma (TSA), or hyperplastic polyp (HP)] divided by total patients/colonoscopies. Prevalence of SSLs excluded TSAs and HPs from the analysis. SPDR was the number of colonoscopies detecting one or more SP divided by total colonoscopies. SSLDR was calculated similarly but focused on SSLs only. Other outcomes included
advanced SSLs (SSL with dysplasia or ≥ 10 mm) detection rate, polyps prevenance and detection rates based on location (proximal vs. distal), gender, and FIT threshold. A proportion meta-analysis, utilizing the random effects model, was used to generate the pooled rates with their corresponding 95% confidence intervals (CI). I2 adjudicated the heterogeneity.
Results: Twenty-two studies met the inclusion criteria, involving 513,080 FIT-positive individuals undergoing colonoscopy. The pooled prevalence of SPs was 19.4% (95% CI: 16.5%–22.8%, I² = 99.747%), with a pooled SPDR of 12.7% (95% CI: 8.7%–18.3%, I² = 99.913%) (Men: 3.8%, and women: 4.2%). For SSLs, the overall pooled prevalence was 7.7% (95% CI: 6.2%–9.5%, I² = 99.415%), with a pooled SSLDR of 4.3% (95% CI: 3.4%–5.5%, I² = 99.586%) (Men: 4.4% and Women 4.4%) (Proximal SSLDR: 1.6%, and distal SSLDR 1%). The overall pooled prevalence of detected advanced SSLs was 7% (95%CI: 2.1%–3.5%, I² = 94.076%), while pooled advanced SSLDR was 1.4% (95% CI: 1 %– 1.9%, I² = 97.024%). Table 1 summarizes the results for SPDR and SSLDR, stratified by location, gender, FIT threshold, and the country of origin of the studies.
Discussion: Our analysis provides valuable information regarding SSL detection rates in FIT-positive individuals which can be used as a quality benchmark in FIT-based population screening programs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Fouad Jaber indicated no relevant financial relationships.
Mohammad Jaber indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Tala Alsharaeh indicated no relevant financial relationships.
Abdelrahman Mohamed Mahmoud indicated no relevant financial relationships.
Anas Alselek indicated no relevant financial relationships.
Yazan Abboud indicated no relevant financial relationships.
Mouhand F.H. Mohamed indicated no relevant financial relationships.
Abubaker O. Abdalla indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Mohamed Abdallah indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Aasma Shaukat: iterative health; Freenome – Consultant.
Fouad Jaber, MD, MS1, Mohammad Jaber, MD2, Saqr Alsakarneh, MD1, Tala Alsharaeh, MD3, Abdelrahman Mohamed Mahmoud, MD4, Anas Alselek, MD5, Yazan Abboud, MD6, Mouhand F.H. Mohamed, MD7, Abubaker O. Abdalla, MD8, Khalid Ahmed, MD9, Mohamed Abdallah, MD10, Mohammad Bilal, MD11, Aasma Shaukat, MD, MPH12. P3649 - Prevalence and Detection Rates of Serrated Polyps and Sessile Serrated Lesions in Average Risk Persons With Positive Fecal Immunohistochemical Test Undergoing Colonoscopy: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
