Tuesday Poster Session
Category: Colon
P3730 - Cronkhite-Canada Syndrome Presenting as Severe Protein-Losing Enteropathy: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nabil El Hage Chehade, MD
Scripps Clinic
San Diego, CA
Presenting Author(s)
Nabil El Hage Chehade, MD1, Olivia Lanser, MD2, Rohit Khanna, DO3, Vandan Patel, MD1, Joy-Marie Hermes, MD4, Fei Bao, MD1, Gordon Liss, MD5, John Lyons, MD5, Gauree Konijeti, MD, MPH5
1Scripps Clinic, San Diego, CA; 2Scripps Green Hospital, La Jolla, CA; 3Scripps Green Hospital, San Diego, CA; 4Scripps Clinic & Scripps Research Institute, San Diego, CA; 5Scripps Clinic, La Jolla, CA
Introduction: Cronkhite-Canada syndrome (CCS) is a rare, non-familial disorder associated with severe diarrhea, weight loss, and gastrointestinal (GI) polyposis. CCS carries a high mortality and malignant transformation rate with death often due to GI bleeding, sepsis, and congestive heart failure. We present a case of CCS manifesting as protein-losing enteropathy causing severe electrolyte disturbances and sarcopenia.
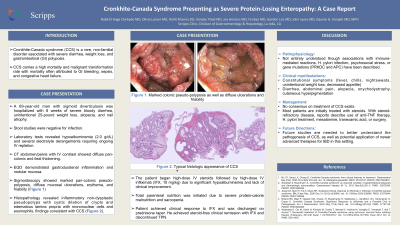
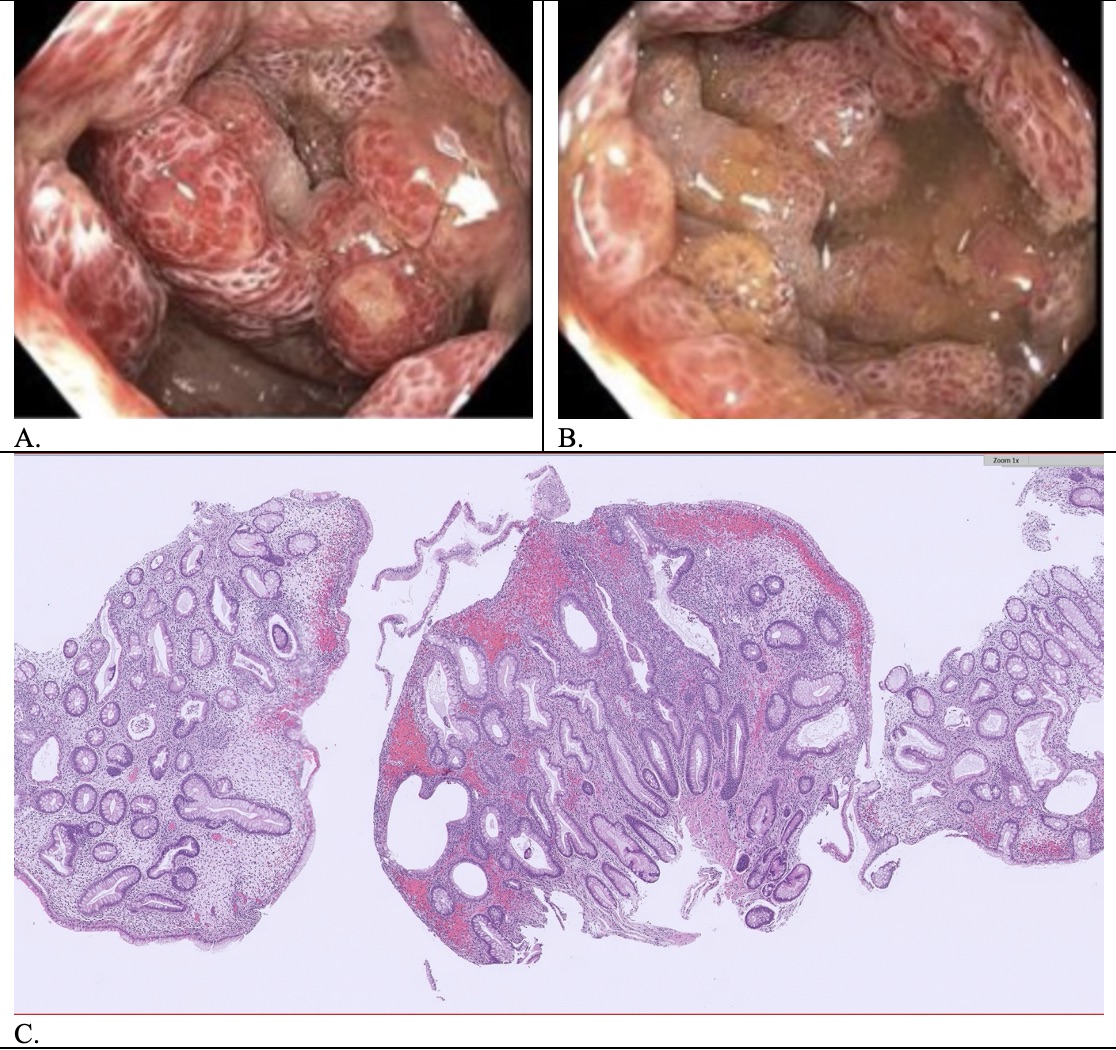
Case Description/Methods: A 69-year-old man with sigmoid diverticulosis was hospitalized with 8 weeks of severe bloody diarrhea, unintentional 25-pound weight loss, alopecia, and nail atrophy. Stool studies were negative for infection. Labs revealed hypoalbuminemia (2.0 g/dL) and several electrolyte derangements requiring ongoing IV repletion. CT abdomen/pelvis with IV contrast showed diffuse pan-colonic and ileal thickening. Sigmoidoscopy showed marked pan-colonic pseudo-polyposis, diffuse mucosal ulcerations, erythema, and friability. EGD demonstrated gastroduodenal gastritis and nodular mucosa. Histopathology revealed inflammatory non-dysplastic pseudopolyps with cystically dilated crypts and edematous lamina propria with mononuclear cells and eosinophils, consistent with CCS. The patient began high-dose IV steroids followed by high-dose IV infliximab (IFX, 10 mg/kg) due to lack of clinical improvement and significant hypoalbuminemia. Total parenteral nutrition was initiated due to severe protein-calorie malnutrition and sarcopenia. Patient achieved clinical response to IFX and was discharged on prednisone taper. He achieved steroid-free clinical remission with IFX and discontinued TPN.
Discussion: The pathophysiology of CCS is not clear, though associations with immune-mediated reactions, H. pylori infection, psychosocial stress, or gene mutations (PRKDC and APC) have been described. No consensus on treatment of CCS exists, and most patients are initially treated with steroids. With steroid-refractory disease, reports describe use of anti-TNF therapy, H. pylori treatment, mesalamine, tranexamic acid, or surgery. Fortunately, our patient responded well to IFX. Future studies are needed to better understand the pathogenesis of CCS, as well as potential application of newer advanced therapies for IBD in this setting.
Disclosures:
Nabil El Hage Chehade, MD1, Olivia Lanser, MD2, Rohit Khanna, DO3, Vandan Patel, MD1, Joy-Marie Hermes, MD4, Fei Bao, MD1, Gordon Liss, MD5, John Lyons, MD5, Gauree Konijeti, MD, MPH5. P3730 - Cronkhite-Canada Syndrome Presenting as Severe Protein-Losing Enteropathy: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Scripps Clinic, San Diego, CA; 2Scripps Green Hospital, La Jolla, CA; 3Scripps Green Hospital, San Diego, CA; 4Scripps Clinic & Scripps Research Institute, San Diego, CA; 5Scripps Clinic, La Jolla, CA
Introduction: Cronkhite-Canada syndrome (CCS) is a rare, non-familial disorder associated with severe diarrhea, weight loss, and gastrointestinal (GI) polyposis. CCS carries a high mortality and malignant transformation rate with death often due to GI bleeding, sepsis, and congestive heart failure. We present a case of CCS manifesting as protein-losing enteropathy causing severe electrolyte disturbances and sarcopenia.
Case Description/Methods: A 69-year-old man with sigmoid diverticulosis was hospitalized with 8 weeks of severe bloody diarrhea, unintentional 25-pound weight loss, alopecia, and nail atrophy. Stool studies were negative for infection. Labs revealed hypoalbuminemia (2.0 g/dL) and several electrolyte derangements requiring ongoing IV repletion. CT abdomen/pelvis with IV contrast showed diffuse pan-colonic and ileal thickening. Sigmoidoscopy showed marked pan-colonic pseudo-polyposis, diffuse mucosal ulcerations, erythema, and friability. EGD demonstrated gastroduodenal gastritis and nodular mucosa. Histopathology revealed inflammatory non-dysplastic pseudopolyps with cystically dilated crypts and edematous lamina propria with mononuclear cells and eosinophils, consistent with CCS. The patient began high-dose IV steroids followed by high-dose IV infliximab (IFX, 10 mg/kg) due to lack of clinical improvement and significant hypoalbuminemia. Total parenteral nutrition was initiated due to severe protein-calorie malnutrition and sarcopenia. Patient achieved clinical response to IFX and was discharged on prednisone taper. He achieved steroid-free clinical remission with IFX and discontinued TPN.
Discussion: The pathophysiology of CCS is not clear, though associations with immune-mediated reactions, H. pylori infection, psychosocial stress, or gene mutations (PRKDC and APC) have been described. No consensus on treatment of CCS exists, and most patients are initially treated with steroids. With steroid-refractory disease, reports describe use of anti-TNF therapy, H. pylori treatment, mesalamine, tranexamic acid, or surgery. Fortunately, our patient responded well to IFX. Future studies are needed to better understand the pathogenesis of CCS, as well as potential application of newer advanced therapies for IBD in this setting.
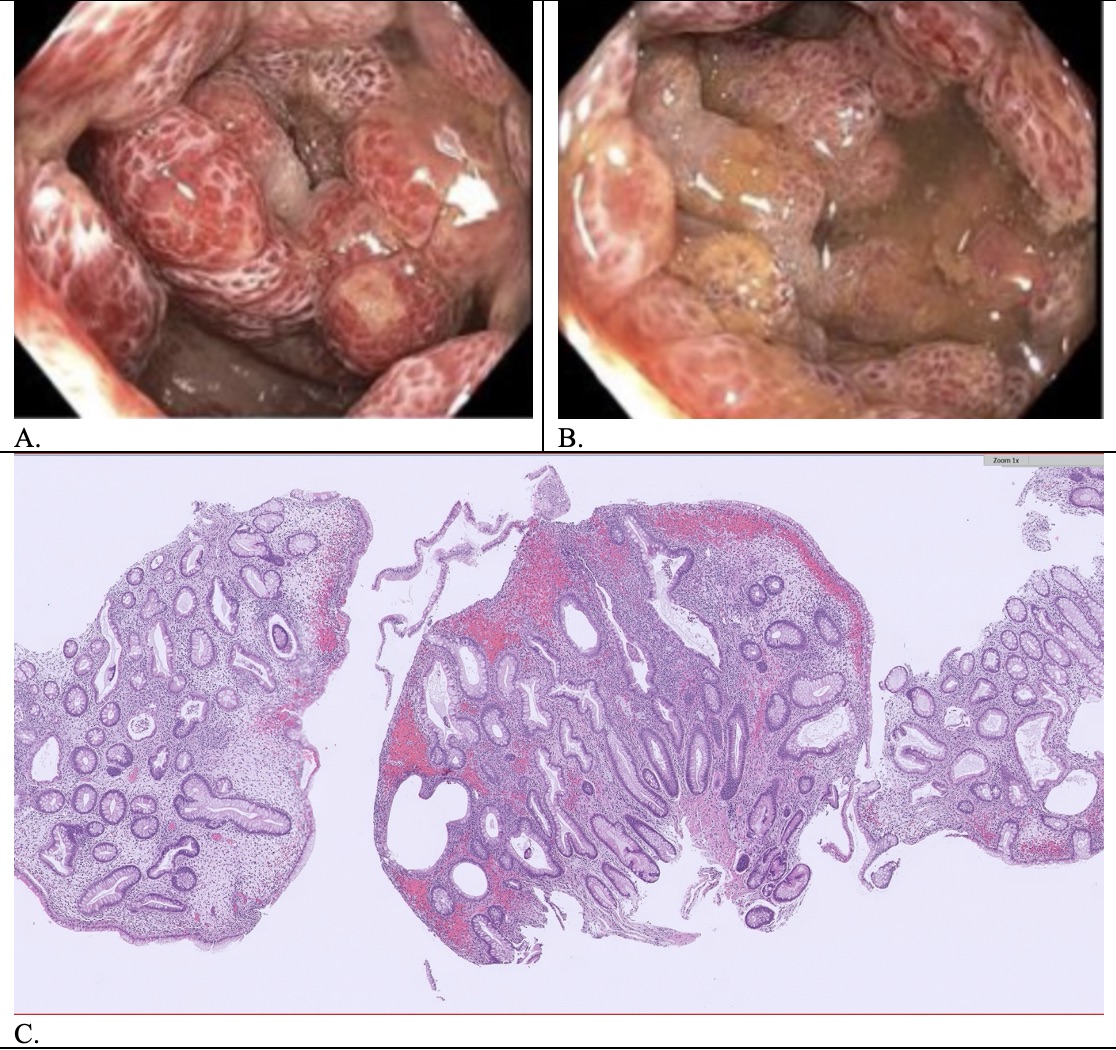
Figure: (A-B) Sigmoidoscopy showing marked pan-colonic pseudo-polyposis, diffuse mucosal ulcerations, erythema and friability; (C) Histopathology demonstrating inflammatory non-dysplastic pseudopolyps with cystically dilated crypts and edematous lamina propria with mononuclear cells and eosinophils, consistent with CCS
Disclosures:
Nabil El Hage Chehade indicated no relevant financial relationships.
Olivia Lanser indicated no relevant financial relationships.
Rohit Khanna indicated no relevant financial relationships.
Vandan Patel indicated no relevant financial relationships.
Joy-Marie Hermes indicated no relevant financial relationships.
Fei Bao indicated no relevant financial relationships.
Gordon Liss indicated no relevant financial relationships.
John Lyons indicated no relevant financial relationships.
Gauree Konijeti: Abbvie – Advisory Committee/Board Member, Consultant. Lilly – Consultant, Speakers Bureau. Pfizer – Advisory Committee/Board Member. Takeda – Speakers Bureau.
Nabil El Hage Chehade, MD1, Olivia Lanser, MD2, Rohit Khanna, DO3, Vandan Patel, MD1, Joy-Marie Hermes, MD4, Fei Bao, MD1, Gordon Liss, MD5, John Lyons, MD5, Gauree Konijeti, MD, MPH5. P3730 - Cronkhite-Canada Syndrome Presenting as Severe Protein-Losing Enteropathy: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
