Tuesday Poster Session
Category: Colon
P3734 - POSTER WITHDRAWN
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Karthic Drishna Perumal, MD1, Taral Patel, MD2, Omar Brijawi, MD3
1Mount Carmel Health System, Powell, OH; 2Zangmeister Center, Grove City, OH; 3Mount Carmel Health System, Grove City, OH
Introduction: Langerhans cell histiocytosis (LCH) is a rare condition caused by the clonal proliferation of bone-marrow-derived antigen-presenting Langerhans cells. In adults, LCH most commonly presents with osseous lesions and less commonly with systemic manifestations. LCH in the gastrointestinal (GI) tract is exceedingly rare with the prevalence limited to only a handful of cases–-approximately less than 30 cases in the English literature to date to the best of our knowledge. We present yet another rare case of Langerhans cell histiocytosis incidentally discovered in the GI tract of an adult and attempt to elucidate further the limited data available on diagnosis, management, and potential treatment of GI LCH.
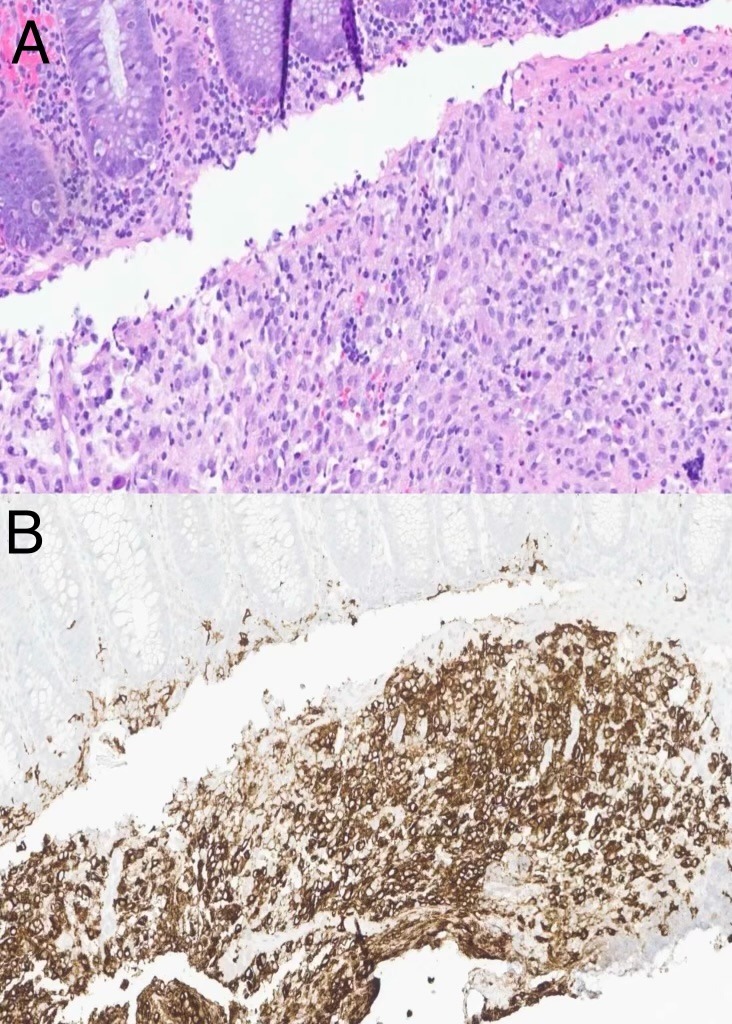
Case Description/Methods: A 44-year-old Caucasian female with a past medical history significant for GERD, type 2 diabetes mellitus, gastroparesis, and a family history of colon cancer was referred for evaluation of chronic intermittent abdominal pain and diarrhea via colonoscopy. The patient denied any hematochezia, constipation, tenesmus, nausea or vomiting with oral intake, unintentional weight loss, or recent sick contacts/illnesses. A colonoscopy showed ulceration in the transverse colon and a biopsy revealed a submucosal infiltrate of Langerhans cells with indented nuclei, pale eosinophilic cytoplasm, and admixed inflammatory cells. Furthermore, immunohistochemical staining revealed cells strongly positive for S-100 protein, CD-1a, and CD56–confirming the diagnosis of LCH.
Discussion: Langerhans cells within the skin that play a key role in the sentinel detection of foreign antigens. The malignancy of this disease comes from the myeloid progenitors in the bone marrow instead of the skin. Singhi et al. studied 24 cases in which GI LCH was observed predominantly in the pediatric population and only a handful of adult cases, predominantly female. The majority of cases occurring in the lower GI tract were found in the sigmoid colon, and presented as an isolated colonic polyp found on endoscopy. Our patient presented with a transverse colonic ulcer–a location with one of the least occurring cases in the lower GI tract. Individuals can have a limited disease that often requires observation or local resection, but those afflicted with multisystem involvement require chemotherapy. Due to the rarity of cases, future studies and trials will be paramount in narrowing down the disease’s predilection for certain presentations such as the GI tract and potential treatment as well.
Disclosures:
Karthic Drishna Perumal, MD1, Taral Patel, MD2, Omar Brijawi, MD3. P3734 - POSTER WITHDRAWN, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Carmel Health System, Powell, OH; 2Zangmeister Center, Grove City, OH; 3Mount Carmel Health System, Grove City, OH
Introduction: Langerhans cell histiocytosis (LCH) is a rare condition caused by the clonal proliferation of bone-marrow-derived antigen-presenting Langerhans cells. In adults, LCH most commonly presents with osseous lesions and less commonly with systemic manifestations. LCH in the gastrointestinal (GI) tract is exceedingly rare with the prevalence limited to only a handful of cases–-approximately less than 30 cases in the English literature to date to the best of our knowledge. We present yet another rare case of Langerhans cell histiocytosis incidentally discovered in the GI tract of an adult and attempt to elucidate further the limited data available on diagnosis, management, and potential treatment of GI LCH.
Case Description/Methods: A 44-year-old Caucasian female with a past medical history significant for GERD, type 2 diabetes mellitus, gastroparesis, and a family history of colon cancer was referred for evaluation of chronic intermittent abdominal pain and diarrhea via colonoscopy. The patient denied any hematochezia, constipation, tenesmus, nausea or vomiting with oral intake, unintentional weight loss, or recent sick contacts/illnesses. A colonoscopy showed ulceration in the transverse colon and a biopsy revealed a submucosal infiltrate of Langerhans cells with indented nuclei, pale eosinophilic cytoplasm, and admixed inflammatory cells. Furthermore, immunohistochemical staining revealed cells strongly positive for S-100 protein, CD-1a, and CD56–confirming the diagnosis of LCH.
Discussion: Langerhans cells within the skin that play a key role in the sentinel detection of foreign antigens. The malignancy of this disease comes from the myeloid progenitors in the bone marrow instead of the skin. Singhi et al. studied 24 cases in which GI LCH was observed predominantly in the pediatric population and only a handful of adult cases, predominantly female. The majority of cases occurring in the lower GI tract were found in the sigmoid colon, and presented as an isolated colonic polyp found on endoscopy. Our patient presented with a transverse colonic ulcer–a location with one of the least occurring cases in the lower GI tract. Individuals can have a limited disease that often requires observation or local resection, but those afflicted with multisystem involvement require chemotherapy. Due to the rarity of cases, future studies and trials will be paramount in narrowing down the disease’s predilection for certain presentations such as the GI tract and potential treatment as well.
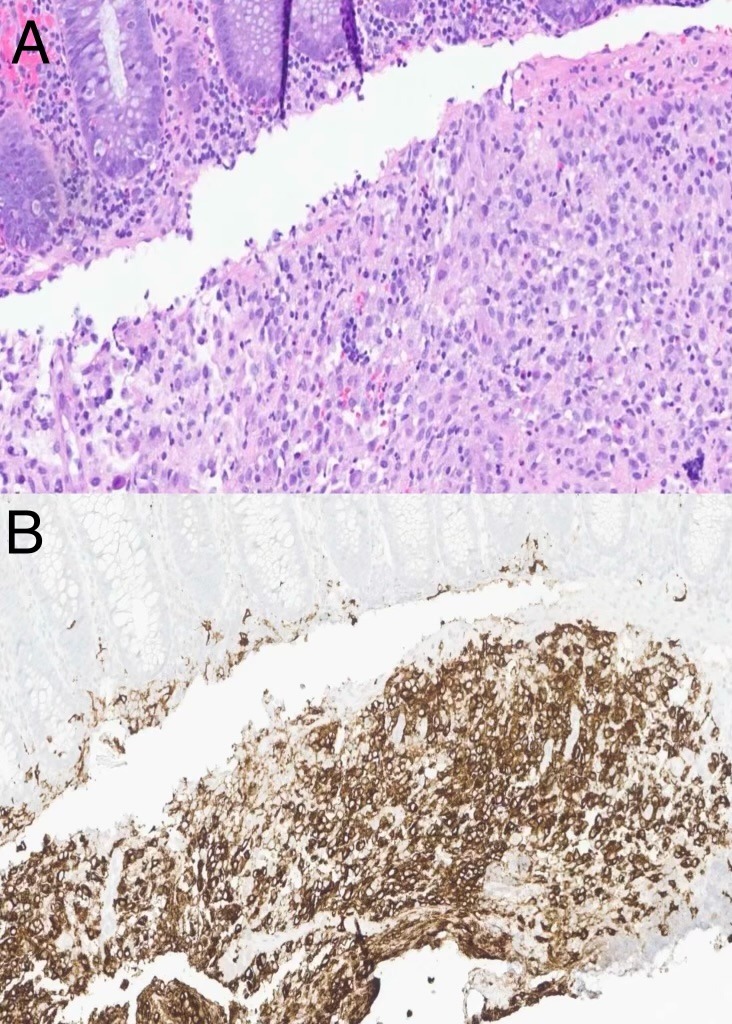
Figure: A) Transverse colon biopsy with histiocytic infiltrate in the lamina propria
B) CD-1a+ immunohistochemical staining of colon biopsy
B) CD-1a+ immunohistochemical staining of colon biopsy
Disclosures:
Karthic Drishna Perumal indicated no relevant financial relationships.
Taral Patel indicated no relevant financial relationships.
Omar Brijawi indicated no relevant financial relationships.
Karthic Drishna Perumal, MD1, Taral Patel, MD2, Omar Brijawi, MD3. P3734 - POSTER WITHDRAWN, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
