Tuesday Poster Session
Category: Colon
P3735 - When the Casual Colonoscopy Catches the Crazy: Is it Crohn’s or Something Else
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jasmine Tidwell, MD
UConn John Dempsey Hospital
Hartford, CT
Presenting Author(s)
Jasmine Tidwell, MD1, Sarah Canavan, MD2
1UConn John Dempsey Hospital, Hartford, CT; 2CT GI, Waterford, CT
Introduction: GI tuberculosis (GITB) is a leading cause of extrapulmonary TB. Due to the limited accuracy of diagnostic tests and the overlap of symptoms with other GI diseases, raising awareness is crucial. We present a case of incidentally found Crohn’s versus GITB.
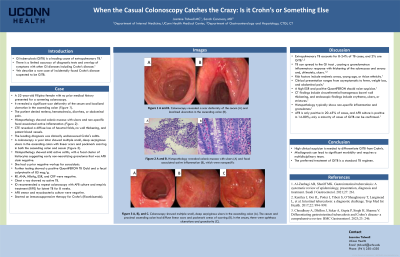
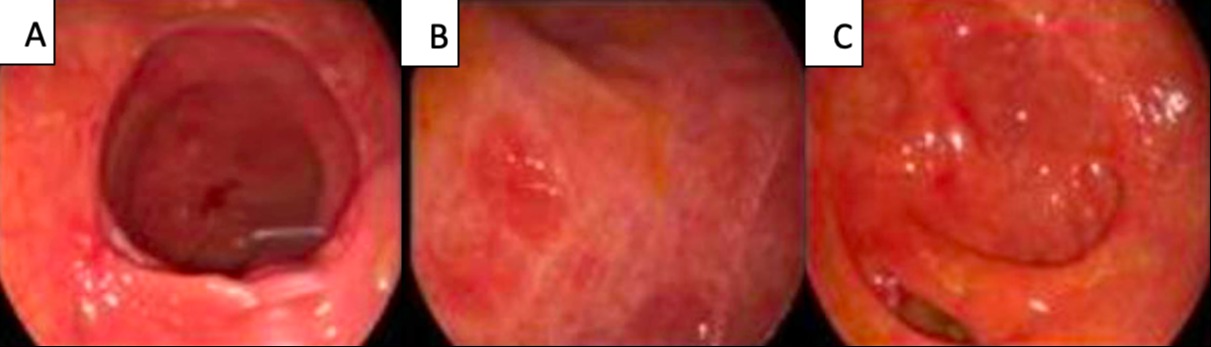
Case Description/Methods: A 52-year-old Filipino female with no prior history underwent a screening colonoscopy, revealing a significant scar deformity of the cecum and localized ulceration in the ascending colon. She denied any symptoms. Histopathology showed colonic mucosa with ulcers and non-specific focal associated active inflammation. A CTE revealed a diffuse loss of haustral folds, no wall thickening, and patent blood vessels. It was believed to be clinically undiscovered Crohn's colitis. Due to a desire to monitor endoscopically, a colonoscopy a year later showed multiple small, deep serpiginous ulcers in the ascending colon with linear scars and pockmark scarring in both the ascending colon and cecum. The cecum also had aphthous ulcerations and granularity. Histopathology showed mild active colitis, with a focal cluster of histiocytes suggesting early non-necrotizing granuloma that was AFB stain negative. She had a prior negative workup for sarcoidosis. Further testing showed a positive QuantiFERON TB Gold and a calprotectin of 85 mcg/g. All other labs were negative, including RF, ANA, HBsAg, ESR, and CRP. Chest x-ray showed no active TB. ID recommended a repeat colonoscopy with AFB culture and empiric treatment for latent TB.
Discussion: Extrapulmonary TB accounts for 8-24% of TB cases, and 2% are GITB. TB can spread to the GI tract via lymphatics, bloodstream, or ingestion, invading the submucosa and causing a granulomatous inflammatory response with thickening of the submucosa and serosa and, ultimately, ulcers. Risk factors include endemic areas, young age, or Asian ethnicity. The clinical presentation ranges from asymptomatic to fever, weight loss, and abdominal pain. A high ESR and positive QuantiFERON should raise suspicion. However, if normal GITB can’t be excluded. CT findings include circumferential homogenous bowel wall thickening, and endoscopic findings include erythema, ulcers, or strictures. Histopathology typically shows non-specific inflammation and granulomas. AFB is only positive in 20-45% of cases and AFB culture in 14-80%; only a minority of cases can be confirmed. Differentiating GITB from Crohn’s can be challenging as there are no pathognomonic features; however, mistreatment can lead to significant morbidity.
Disclosures:
Jasmine Tidwell, MD1, Sarah Canavan, MD2. P3735 - When the Casual Colonoscopy Catches the Crazy: Is it Crohn’s or Something Else, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1UConn John Dempsey Hospital, Hartford, CT; 2CT GI, Waterford, CT
Introduction: GI tuberculosis (GITB) is a leading cause of extrapulmonary TB. Due to the limited accuracy of diagnostic tests and the overlap of symptoms with other GI diseases, raising awareness is crucial. We present a case of incidentally found Crohn’s versus GITB.
Case Description/Methods: A 52-year-old Filipino female with no prior history underwent a screening colonoscopy, revealing a significant scar deformity of the cecum and localized ulceration in the ascending colon. She denied any symptoms. Histopathology showed colonic mucosa with ulcers and non-specific focal associated active inflammation. A CTE revealed a diffuse loss of haustral folds, no wall thickening, and patent blood vessels. It was believed to be clinically undiscovered Crohn's colitis. Due to a desire to monitor endoscopically, a colonoscopy a year later showed multiple small, deep serpiginous ulcers in the ascending colon with linear scars and pockmark scarring in both the ascending colon and cecum. The cecum also had aphthous ulcerations and granularity. Histopathology showed mild active colitis, with a focal cluster of histiocytes suggesting early non-necrotizing granuloma that was AFB stain negative. She had a prior negative workup for sarcoidosis. Further testing showed a positive QuantiFERON TB Gold and a calprotectin of 85 mcg/g. All other labs were negative, including RF, ANA, HBsAg, ESR, and CRP. Chest x-ray showed no active TB. ID recommended a repeat colonoscopy with AFB culture and empiric treatment for latent TB.
Discussion: Extrapulmonary TB accounts for 8-24% of TB cases, and 2% are GITB. TB can spread to the GI tract via lymphatics, bloodstream, or ingestion, invading the submucosa and causing a granulomatous inflammatory response with thickening of the submucosa and serosa and, ultimately, ulcers. Risk factors include endemic areas, young age, or Asian ethnicity. The clinical presentation ranges from asymptomatic to fever, weight loss, and abdominal pain. A high ESR and positive QuantiFERON should raise suspicion. However, if normal GITB can’t be excluded. CT findings include circumferential homogenous bowel wall thickening, and endoscopic findings include erythema, ulcers, or strictures. Histopathology typically shows non-specific inflammation and granulomas. AFB is only positive in 20-45% of cases and AFB culture in 14-80%; only a minority of cases can be confirmed. Differentiating GITB from Crohn’s can be challenging as there are no pathognomonic features; however, mistreatment can lead to significant morbidity.
Figure: Fig 1 A, B, C. Colonoscopy showed multiple small, deep serpiginous ulcers in the ascending colon (A). The cecum and proximal ascending colon had diffuse linear scars and pockmark areas of scarring (B). In the cecum, there were aphthous ulcerations and granularity (C).
Disclosures:
Jasmine Tidwell indicated no relevant financial relationships.
Sarah Canavan indicated no relevant financial relationships.
Jasmine Tidwell, MD1, Sarah Canavan, MD2. P3735 - When the Casual Colonoscopy Catches the Crazy: Is it Crohn’s or Something Else, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
