Tuesday Poster Session
Category: Colon
P3737 - Neutropenic Enterocolitis After Single Dose of CAPOX in Newly Diagnosed Colon Cancer
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- BL
Boris Livitz, MD
Stony Brook Southampton Hospital
Patchogue, NY
Presenting Author(s)
Boris Livitz, MD1, Jagraj Singh, DO1, Elnaz Mahbub, DO2, Andrey Moiseyenko, DO1, Rachel Para, 1, Ahsan Khan, MD3
1Stony Brook Southampton Hospital, Southampton, NY; 2Stony Brook Southampton Hospital, Jamaica, NY; 3Stony Brook Medicine, Southampton, NY
Introduction: Neutropenic patients are at an increased risk of severe infections and require a high index of suspicion to prevent poor outcomes. This case illustrates neutropenic enterocolitis (NE) after one round of adjuvant chemotherapy for colon adenocarcinoma.
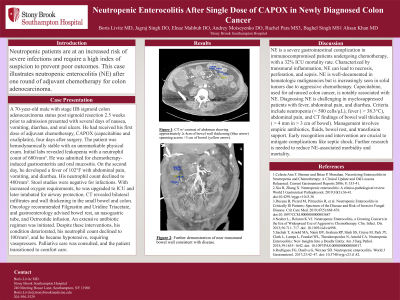
Case Description/Methods: A 70-year-old male with stage IIB sigmoid colon adenocarcinoma status post sigmoid resection 2.5 weeks prior to admission presented with several days of nausea, vomiting, diarrhea, and oral ulcers. He had received his first dose of adjuvant chemotherapy, CAPOX (capecitabine and oxaliplatin), four days after surgery. The patient was hemodynamically stable with an unremarkable physical exam. Initial labs revealed leukopenia with a neutrophil count of 680/mm³. He was admitted for chemotherapy-induced gastroenteritis and oral mucositis. On the second day, he developed a fever of 102°F with abdominal pain, vomiting, and diarrhea. His neutrophil count declined to 480/mm³. Stool studies were negative for infections. With increased oxygen requirements, he was upgraded to ICU and later intubated for airway protection. CT revealed bilateral infiltrates and wall thickening in the small bowel and colon. Oncology recommended Filgrastim and Uridine Triacetate, and gastroenterology advised bowel rest, an nasogastric tube, and Octreotide infusion. An extensive antibiotic regimen was initiated. Despite these interventions, his condition deteriorated, his neutrophil count declined to 100/mm³, and he became hypotensive, requiring vasopressors. Palliative care was consulted, and the patient transitioned to comfort care.
Discussion: NE is a severe gastrointestinal complication in immunocompromised patients undergoing chemotherapy, with a 32% ICU mortality rate. Characterized by transmural inflammation, NE can lead to necrosis, perforation, and sepsis. NE is well-documented in hematologic malignancies but is increasingly seen in solid tumors due to aggressive chemotherapy. Capecitabine, used for advanced colon cancer, is notably associated with NE. Diagnosing NE is challenging in myelosuppressed patients with fever, abdominal pain, and diarrhea. Criteria include neutropenia (< 500 cells/µL), fever ( > 38.3°C), abdominal pain, and CT findings of bowel wall thickening ( > 4 mm in > 3 cm of bowel). Management involves empiric antibiotics, fluids, bowel rest, and transfusion support. Early recognition and intervention are crucial to mitigate complications like septic shock. Further research is needed to reduce NE-associated morbidity and mortality.
Disclosures:
Boris Livitz, MD1, Jagraj Singh, DO1, Elnaz Mahbub, DO2, Andrey Moiseyenko, DO1, Rachel Para, 1, Ahsan Khan, MD3. P3737 - Neutropenic Enterocolitis After Single Dose of CAPOX in Newly Diagnosed Colon Cancer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Stony Brook Southampton Hospital, Southampton, NY; 2Stony Brook Southampton Hospital, Jamaica, NY; 3Stony Brook Medicine, Southampton, NY
Introduction: Neutropenic patients are at an increased risk of severe infections and require a high index of suspicion to prevent poor outcomes. This case illustrates neutropenic enterocolitis (NE) after one round of adjuvant chemotherapy for colon adenocarcinoma.
Case Description/Methods: A 70-year-old male with stage IIB sigmoid colon adenocarcinoma status post sigmoid resection 2.5 weeks prior to admission presented with several days of nausea, vomiting, diarrhea, and oral ulcers. He had received his first dose of adjuvant chemotherapy, CAPOX (capecitabine and oxaliplatin), four days after surgery. The patient was hemodynamically stable with an unremarkable physical exam. Initial labs revealed leukopenia with a neutrophil count of 680/mm³. He was admitted for chemotherapy-induced gastroenteritis and oral mucositis. On the second day, he developed a fever of 102°F with abdominal pain, vomiting, and diarrhea. His neutrophil count declined to 480/mm³. Stool studies were negative for infections. With increased oxygen requirements, he was upgraded to ICU and later intubated for airway protection. CT revealed bilateral infiltrates and wall thickening in the small bowel and colon. Oncology recommended Filgrastim and Uridine Triacetate, and gastroenterology advised bowel rest, an nasogastric tube, and Octreotide infusion. An extensive antibiotic regimen was initiated. Despite these interventions, his condition deteriorated, his neutrophil count declined to 100/mm³, and he became hypotensive, requiring vasopressors. Palliative care was consulted, and the patient transitioned to comfort care.
Discussion: NE is a severe gastrointestinal complication in immunocompromised patients undergoing chemotherapy, with a 32% ICU mortality rate. Characterized by transmural inflammation, NE can lead to necrosis, perforation, and sepsis. NE is well-documented in hematologic malignancies but is increasingly seen in solid tumors due to aggressive chemotherapy. Capecitabine, used for advanced colon cancer, is notably associated with NE. Diagnosing NE is challenging in myelosuppressed patients with fever, abdominal pain, and diarrhea. Criteria include neutropenia (< 500 cells/µL), fever ( > 38.3°C), abdominal pain, and CT findings of bowel wall thickening ( > 4 mm in > 3 cm of bowel). Management involves empiric antibiotics, fluids, bowel rest, and transfusion support. Early recognition and intervention are crucial to mitigate complications like septic shock. Further research is needed to reduce NE-associated morbidity and mortality.
Disclosures:
Boris Livitz indicated no relevant financial relationships.
Jagraj Singh indicated no relevant financial relationships.
Elnaz Mahbub indicated no relevant financial relationships.
Andrey Moiseyenko indicated no relevant financial relationships.
Rachel Para indicated no relevant financial relationships.
Ahsan Khan indicated no relevant financial relationships.
Boris Livitz, MD1, Jagraj Singh, DO1, Elnaz Mahbub, DO2, Andrey Moiseyenko, DO1, Rachel Para, 1, Ahsan Khan, MD3. P3737 - Neutropenic Enterocolitis After Single Dose of CAPOX in Newly Diagnosed Colon Cancer, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
