Tuesday Poster Session
Category: Colon
P3752 - Vitamin E Supplementation in Brown Bowel Syndrome: A Case of Diagnostic Challenge and Therapeutic Success
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Muhammad Jahanzaib Khan, MD
Mather Hospital, Northwell Health
New York, NY
Presenting Author(s)
Asfand Bangash, MD1, Muhammad Abdurrahman Butt, MBBS2, Muhammad Jahanzaib Khan, MD3, Hassan Waseem, MBBS4, Abdul Wasaay Khurram, MBBS2
1Shifa International Hospital, Islamabad, Islamabad, Pakistan; 2Shifa College of Medicine, Islamabad, Islamabad, Pakistan; 3Mather Hospital, Northwell Health, New York, NY; 4Shifa College of Medicine, Islamabad, Federally Administered Tribal Areas, Pakistan
Introduction: Brown Bowel Syndrome (BBS), also known as intestinal lipofuscinosis, is a rare gastrointestinal condition characterized by the deposition of lipofuscin within the smooth muscle cells of the bowel. This condition often leads to deficiencies in fat-soluble vitamins, particularly vitamin E, which serves as a potent antioxidant. Vitamin E deficiency not only imparts a brownish discoloration to the bowel wall but also disrupts normal bowel function, potentially leading to severe complications such as intestinal dilation and malabsorption. Presenting this case is relevant for highlighting the diagnostic challenges and effective management strategies for BBS, which can aid physicians encountering similar clinical scenarios.
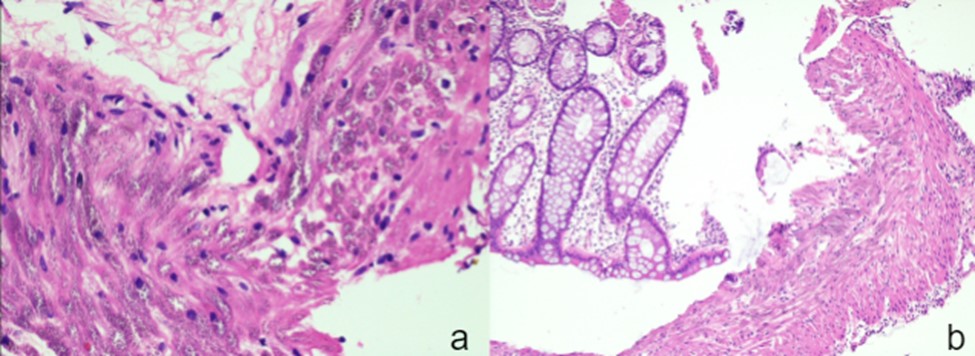
Case Description/Methods: A 27-year-old male with congenital speech and hearing impairment presented with a three-month history of diarrhea, significant weight loss (12 kg), and generalized weakness. His medical history included congenital bowel obstruction and subsequent bowel resection. Upon presentation, the patient appeared cachectic and pale, with notable clubbing of the fingers. Laboratory tests revealed severe hypokalemia and Vitamin E deficiency, both of which were corrected during admission. A CT scan revealed a dilated colon. Sigmoidoscopy showed normal rectal mucosa and an uninflamed anastomosis 10 cm from the anal verge. Biopsies from the proximal anastomosis site showed brownish granules in the muscularis propria, consistent with BBS as shown in Figure 1 (a & b). The patient was discharged on Vitamin E supplements and received counseling on electrolyte replacement. Follow-up showed the patient to be asymptomatic.
Discussion: This case highlights the diagnostic challenge of BBS due to its rarity and nonspecific symptoms. Despite unremarkable initial endoscopic findings, biopsies from the anastomosis site revealed lipofuscin deposits, confirming the diagnosis of BBS. Management involved conservative treatment, with Vitamin E supplementation playing a critical role. This significantly improved the patient's diarrhea and other symptoms. The case illustrates the importance of histopathology in diagnosing BBS and demonstrates the effectiveness of Vitamin E supplementation in symptom management. Key lessons include maintaining a high suspicion for BBS in patients with malabsorption and unexplained gastrointestinal symptoms, and recognizing the therapeutic potential of Vitamin E supplementation.
Disclosures:
Asfand Bangash, MD1, Muhammad Abdurrahman Butt, MBBS2, Muhammad Jahanzaib Khan, MD3, Hassan Waseem, MBBS4, Abdul Wasaay Khurram, MBBS2. P3752 - Vitamin E Supplementation in Brown Bowel Syndrome: A Case of Diagnostic Challenge and Therapeutic Success, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Shifa International Hospital, Islamabad, Islamabad, Pakistan; 2Shifa College of Medicine, Islamabad, Islamabad, Pakistan; 3Mather Hospital, Northwell Health, New York, NY; 4Shifa College of Medicine, Islamabad, Federally Administered Tribal Areas, Pakistan
Introduction: Brown Bowel Syndrome (BBS), also known as intestinal lipofuscinosis, is a rare gastrointestinal condition characterized by the deposition of lipofuscin within the smooth muscle cells of the bowel. This condition often leads to deficiencies in fat-soluble vitamins, particularly vitamin E, which serves as a potent antioxidant. Vitamin E deficiency not only imparts a brownish discoloration to the bowel wall but also disrupts normal bowel function, potentially leading to severe complications such as intestinal dilation and malabsorption. Presenting this case is relevant for highlighting the diagnostic challenges and effective management strategies for BBS, which can aid physicians encountering similar clinical scenarios.
Case Description/Methods: A 27-year-old male with congenital speech and hearing impairment presented with a three-month history of diarrhea, significant weight loss (12 kg), and generalized weakness. His medical history included congenital bowel obstruction and subsequent bowel resection. Upon presentation, the patient appeared cachectic and pale, with notable clubbing of the fingers. Laboratory tests revealed severe hypokalemia and Vitamin E deficiency, both of which were corrected during admission. A CT scan revealed a dilated colon. Sigmoidoscopy showed normal rectal mucosa and an uninflamed anastomosis 10 cm from the anal verge. Biopsies from the proximal anastomosis site showed brownish granules in the muscularis propria, consistent with BBS as shown in Figure 1 (a & b). The patient was discharged on Vitamin E supplements and received counseling on electrolyte replacement. Follow-up showed the patient to be asymptomatic.
Discussion: This case highlights the diagnostic challenge of BBS due to its rarity and nonspecific symptoms. Despite unremarkable initial endoscopic findings, biopsies from the anastomosis site revealed lipofuscin deposits, confirming the diagnosis of BBS. Management involved conservative treatment, with Vitamin E supplementation playing a critical role. This significantly improved the patient's diarrhea and other symptoms. The case illustrates the importance of histopathology in diagnosing BBS and demonstrates the effectiveness of Vitamin E supplementation in symptom management. Key lessons include maintaining a high suspicion for BBS in patients with malabsorption and unexplained gastrointestinal symptoms, and recognizing the therapeutic potential of Vitamin E supplementation.
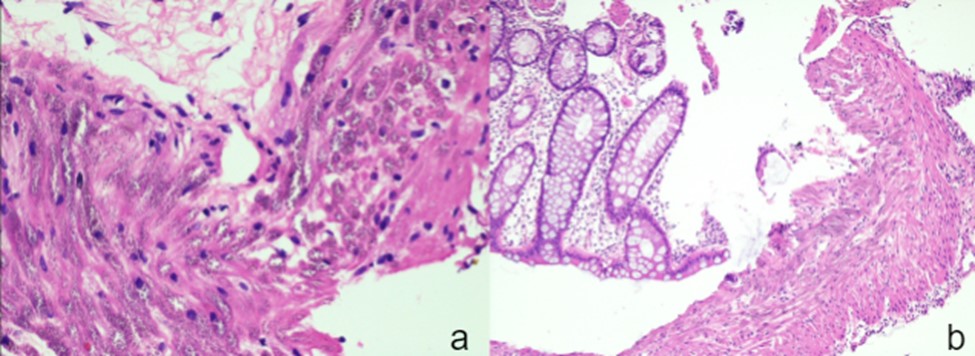
Figure: Figure 1 (a & b)
Disclosures:
Asfand Bangash indicated no relevant financial relationships.
Muhammad Abdurrahman Butt indicated no relevant financial relationships.
Muhammad Jahanzaib Khan indicated no relevant financial relationships.
Hassan Waseem indicated no relevant financial relationships.
Abdul Wasaay Khurram indicated no relevant financial relationships.
Asfand Bangash, MD1, Muhammad Abdurrahman Butt, MBBS2, Muhammad Jahanzaib Khan, MD3, Hassan Waseem, MBBS4, Abdul Wasaay Khurram, MBBS2. P3752 - Vitamin E Supplementation in Brown Bowel Syndrome: A Case of Diagnostic Challenge and Therapeutic Success, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
