Tuesday Poster Session
Category: Colon
P3753 - Uncommon Presentation of Gastrointestinal Histoplasmosis in an Immunocompromised Patient
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Usha Kellampalli, MBBS
Corewell Health
troy, MI
Presenting Author(s)
Usha Kellampalli, MBBS1, Nathanial Bartosek, MD2, Alsadiq Al-Hillan, MD3, Dariusz Lazarczyk, MD1
1Corewell Health, Royal Oak, MI; 2Beaumont Health, Royal Oak, MI; 3Corewell Health William Beaumont University Hospital, Royal Oak, MI
Introduction: Histoplasmosis rarely involves the gastrointestinal (GI) tract, comprising < 1% of all histoplasmosis cases. If present, GI histoplasmosis most commonly involves the colon or terminal ileum of immunocompromised patients presenting with abdominal pain and diarrhea. This case uniquely displays GI Histoplasmosis without symptoms.
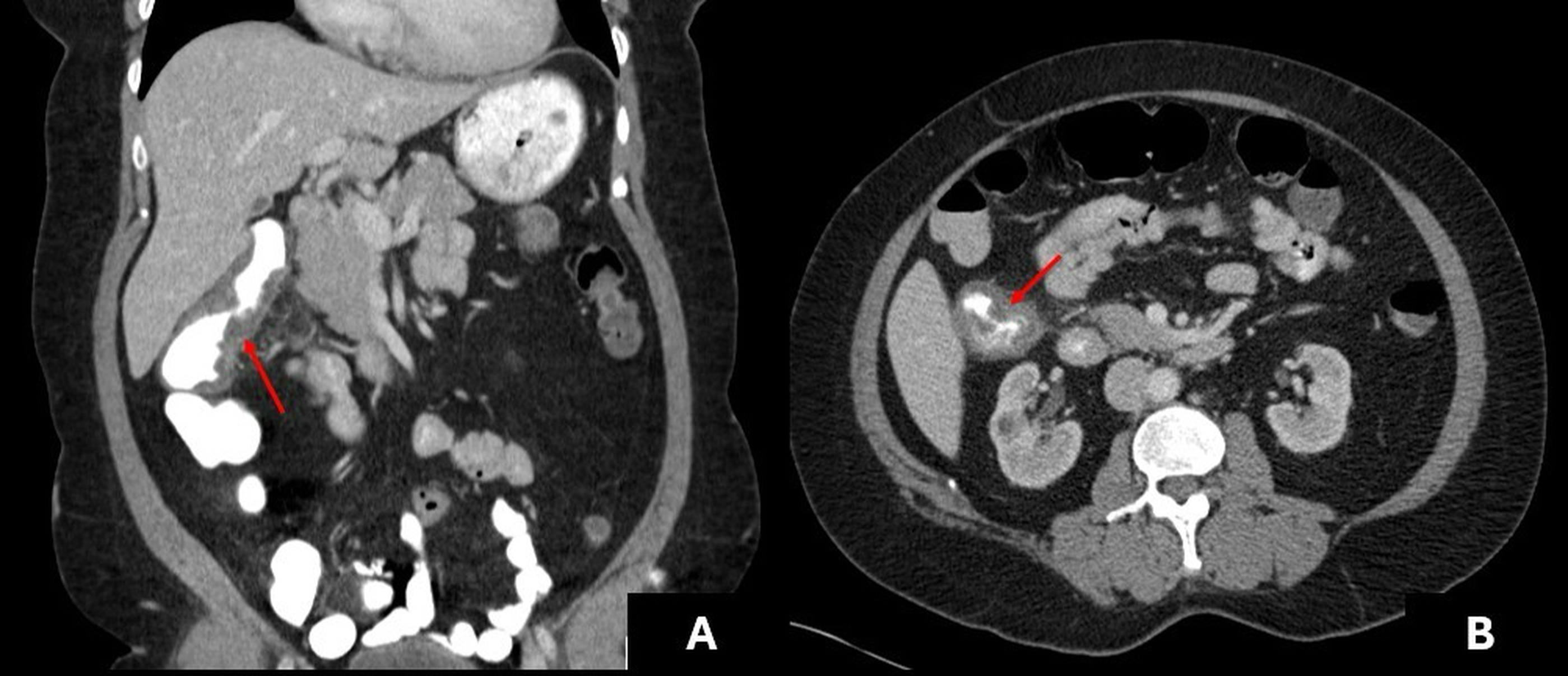
Case Description/Methods: A 51-year-old female with Systemic Lupus Erythematosus on Mycophenolic acid and prednisone underwent a routine screening colonoscopy. The colonoscopy revealed a 3 cm submucosal, ulcerated mass in the distal ascending colon. Biopsies of the lesion showed granulomatous inflammation; tissue stain was consistent with Histoplasmosis. However, urine Histoplasmosis antigen was negative. CT abdomen demonstrated ascending colon colitis with an appreciable mass, correlating with the colonoscopy findings. The patient was initiated on itraconazole for one year. The initial follow-up colonoscopy demonstrated residual findings consistent with colitis and the absence of active disease, with a second follow-up colonoscopy demonstrating resolution of the mass. Urine and serum Histoplasma antigen tested every four weeks for six months maintained to be negative, while the patient was only compliant with four months of therapy.
Discussion: Generally, the presentation of GI Histoplasmosis may include abdominal pain and bloody/non-bloody diarrhea. However, only mild GI symptoms may be present in patients with prominent systemic Histoplasmosis. Diagnosis is proven after biopsy confirmation, with pathologic findings including mucosal ulceration, diffuse lymphohistiocytic infiltration of the bowel wall, submucosal nodules, or polypoid lesions. Early diagnosis and adequate treatment are essential in preventing complications of Histoplasmosis in immunocompromised patients, as disseminated disease may cause severe morbidity and mortality.
This case demonstrates the ability of Histoplasmosis to be asymptomatic with significant GI involvement in immunocompromised hosts. As displayed, it may rarely manifest as a fungal colonic mass, an important concept when examiners perform colonoscopies in at-risk individuals, even with negative urine antigen and serum testing. Continued surveillance of immunocompromised individuals may be warranted, as this case outlines the possibility of further dissemination had it not been discovered earlier. Overall, a high degree of suspicion should be held for multiple infections of the immunocompromised, even when diagnosing colonic masses.
Disclosures:
Usha Kellampalli, MBBS1, Nathanial Bartosek, MD2, Alsadiq Al-Hillan, MD3, Dariusz Lazarczyk, MD1. P3753 - Uncommon Presentation of Gastrointestinal Histoplasmosis in an Immunocompromised Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Corewell Health, Royal Oak, MI; 2Beaumont Health, Royal Oak, MI; 3Corewell Health William Beaumont University Hospital, Royal Oak, MI
Introduction: Histoplasmosis rarely involves the gastrointestinal (GI) tract, comprising < 1% of all histoplasmosis cases. If present, GI histoplasmosis most commonly involves the colon or terminal ileum of immunocompromised patients presenting with abdominal pain and diarrhea. This case uniquely displays GI Histoplasmosis without symptoms.
Case Description/Methods: A 51-year-old female with Systemic Lupus Erythematosus on Mycophenolic acid and prednisone underwent a routine screening colonoscopy. The colonoscopy revealed a 3 cm submucosal, ulcerated mass in the distal ascending colon. Biopsies of the lesion showed granulomatous inflammation; tissue stain was consistent with Histoplasmosis. However, urine Histoplasmosis antigen was negative. CT abdomen demonstrated ascending colon colitis with an appreciable mass, correlating with the colonoscopy findings. The patient was initiated on itraconazole for one year. The initial follow-up colonoscopy demonstrated residual findings consistent with colitis and the absence of active disease, with a second follow-up colonoscopy demonstrating resolution of the mass. Urine and serum Histoplasma antigen tested every four weeks for six months maintained to be negative, while the patient was only compliant with four months of therapy.
Discussion: Generally, the presentation of GI Histoplasmosis may include abdominal pain and bloody/non-bloody diarrhea. However, only mild GI symptoms may be present in patients with prominent systemic Histoplasmosis. Diagnosis is proven after biopsy confirmation, with pathologic findings including mucosal ulceration, diffuse lymphohistiocytic infiltration of the bowel wall, submucosal nodules, or polypoid lesions. Early diagnosis and adequate treatment are essential in preventing complications of Histoplasmosis in immunocompromised patients, as disseminated disease may cause severe morbidity and mortality.
This case demonstrates the ability of Histoplasmosis to be asymptomatic with significant GI involvement in immunocompromised hosts. As displayed, it may rarely manifest as a fungal colonic mass, an important concept when examiners perform colonoscopies in at-risk individuals, even with negative urine antigen and serum testing. Continued surveillance of immunocompromised individuals may be warranted, as this case outlines the possibility of further dissemination had it not been discovered earlier. Overall, a high degree of suspicion should be held for multiple infections of the immunocompromised, even when diagnosing colonic masses.
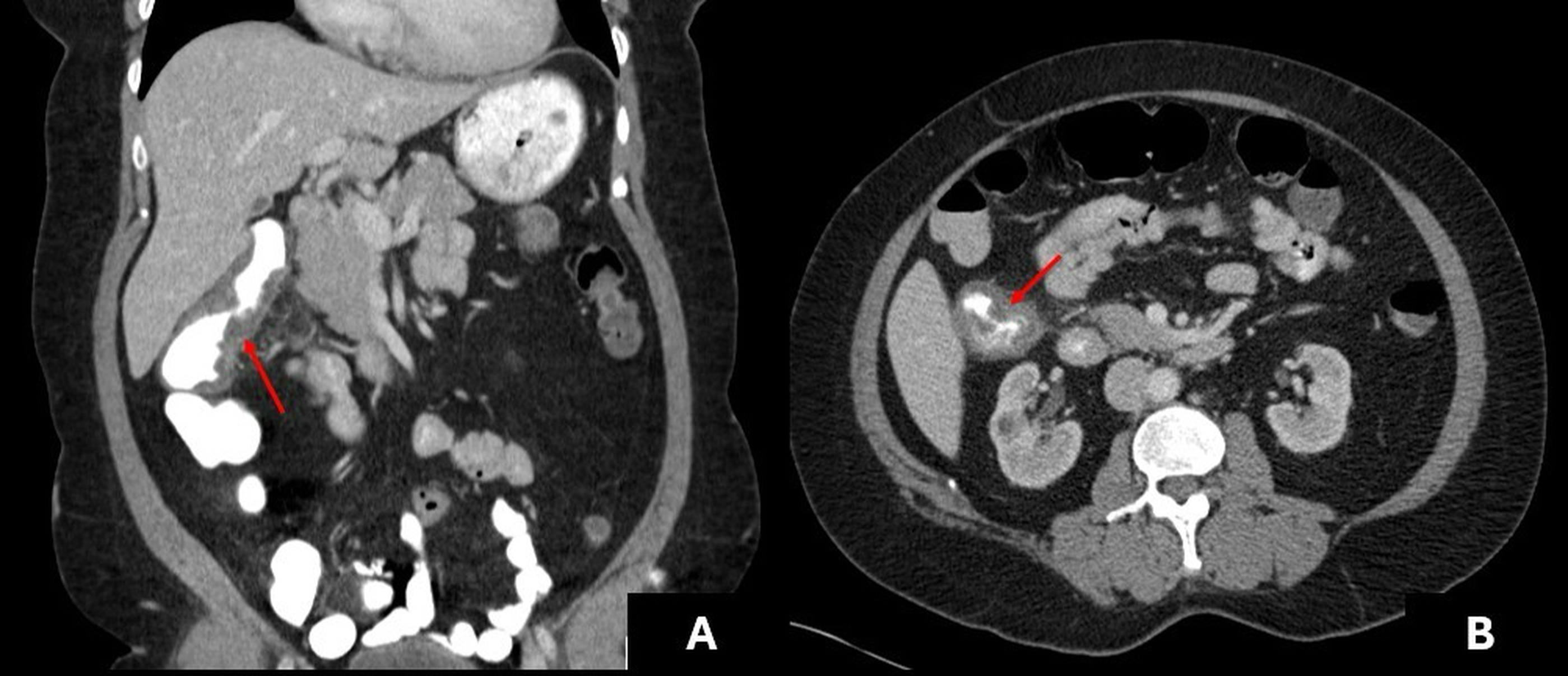
Figure: Mass like lesion and colitis (Red Arrows) noted on (A) Coronal and (B) Transverse view of Computed Tomography (CT) scan with oral contrast, demonstrating the area of concern identified on colonoscopy.
Disclosures:
Usha Kellampalli indicated no relevant financial relationships.
Nathanial Bartosek indicated no relevant financial relationships.
Alsadiq Al-Hillan indicated no relevant financial relationships.
Dariusz Lazarczyk indicated no relevant financial relationships.
Usha Kellampalli, MBBS1, Nathanial Bartosek, MD2, Alsadiq Al-Hillan, MD3, Dariusz Lazarczyk, MD1. P3753 - Uncommon Presentation of Gastrointestinal Histoplasmosis in an Immunocompromised Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
