Tuesday Poster Session
Category: Colon
P3757 - Systemic Mastocytosis and the Pivotal Role of the Gastroenterologist
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SF
Shannon Fernando, BA
Sidney Kimmel Medical College at Thomas Jefferson University
Philadelphia, PA
Presenting Author(s)
Shannon Fernando, BA1, Priya Sehgal, MD, MS, MPH2
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA
Introduction: This case highlights the gastrointestinal (GI) clinical manifestations of systemic mastocytosis (SM). It also emphasizes the importance of colon cancer screening among SM patients.
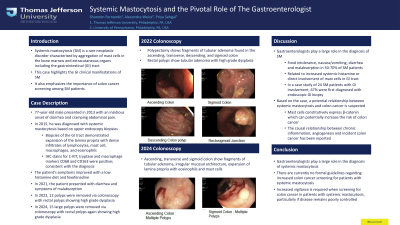
Case Description/Methods: A 77 year old male with no past medical history presented in 2013 with an insidious onset of diarrhea and cramping abdominal pain. He was diagnosed in 2015 with systemic mastocytosis based on upper endoscopy biopsies. Biopsies of the GI tract indicated expansion of the lamina propria with dense infiltrates of lymphocytes, mast cells, macrophages and eosinophils. IHC stains for C-KIT, tryptase, and macrophage markers CD68 and CD163 were also positive; consistent with the diagnosis. The patient was treated with a low histamine diet and fexofenadine to which he initially responded with symptom improvement. In 2021, he again began to have GI symptoms including diarrhea, abdominal pain and showed evidence of malabsorption. In 2022, 12 polyps were removed during colonoscopy, with rectal polyps showing high grade of dysplasia. In 2024, 15 large polyps were removed during colonoscopy with rectal polyps again showing high grade dysplasia.
Discussion: Systemic mastocytosis is a rare neoplastic disorder characterized by aggregation of mast cells in the bone marrow and extracutaneous organs including the GI tract. GI symptoms are the second most frequent manifestation presenting as food intolerance, nausea/vomiting, diarrhea and malabsorption in 50-70% of patients. These symptoms are attributable to increased systemic histamine or direct involvement of mast cells in the GI tract. The role of the gastroenterologist in diagnosing SM is critical. In a case study of 24 SM patients with GI involvement, 67% of cases were first diagnosed by endoscopic GI biopsy. Furthermore, mast cells constitutively express β-catenin which can potentially increase the risk of colon cancer. While, to our knowledge, there is no direct evidence that systemic mastocytosis leads to an increased incidence of colon cancer, the causal relationship between chronic inflammation, angiogenesis and incident colon cancer has been reported. There are currently no formal guidelines regarding increased colon cancer screening for patients with systemic mastocytosis. Based on our case, we recommend increased vigilance and attention to detail with regard to screening for colon cancer in patients with systemic mastocytosis particularly if disease remains poorly controlled.
Disclosures:
Shannon Fernando, BA1, Priya Sehgal, MD, MS, MPH2. P3757 - Systemic Mastocytosis and the Pivotal Role of the Gastroenterologist, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 2University of Pennsylvania, Philadelphia, PA
Introduction: This case highlights the gastrointestinal (GI) clinical manifestations of systemic mastocytosis (SM). It also emphasizes the importance of colon cancer screening among SM patients.
Case Description/Methods: A 77 year old male with no past medical history presented in 2013 with an insidious onset of diarrhea and cramping abdominal pain. He was diagnosed in 2015 with systemic mastocytosis based on upper endoscopy biopsies. Biopsies of the GI tract indicated expansion of the lamina propria with dense infiltrates of lymphocytes, mast cells, macrophages and eosinophils. IHC stains for C-KIT, tryptase, and macrophage markers CD68 and CD163 were also positive; consistent with the diagnosis. The patient was treated with a low histamine diet and fexofenadine to which he initially responded with symptom improvement. In 2021, he again began to have GI symptoms including diarrhea, abdominal pain and showed evidence of malabsorption. In 2022, 12 polyps were removed during colonoscopy, with rectal polyps showing high grade of dysplasia. In 2024, 15 large polyps were removed during colonoscopy with rectal polyps again showing high grade dysplasia.
Discussion: Systemic mastocytosis is a rare neoplastic disorder characterized by aggregation of mast cells in the bone marrow and extracutaneous organs including the GI tract. GI symptoms are the second most frequent manifestation presenting as food intolerance, nausea/vomiting, diarrhea and malabsorption in 50-70% of patients. These symptoms are attributable to increased systemic histamine or direct involvement of mast cells in the GI tract. The role of the gastroenterologist in diagnosing SM is critical. In a case study of 24 SM patients with GI involvement, 67% of cases were first diagnosed by endoscopic GI biopsy. Furthermore, mast cells constitutively express β-catenin which can potentially increase the risk of colon cancer. While, to our knowledge, there is no direct evidence that systemic mastocytosis leads to an increased incidence of colon cancer, the causal relationship between chronic inflammation, angiogenesis and incident colon cancer has been reported. There are currently no formal guidelines regarding increased colon cancer screening for patients with systemic mastocytosis. Based on our case, we recommend increased vigilance and attention to detail with regard to screening for colon cancer in patients with systemic mastocytosis particularly if disease remains poorly controlled.
Disclosures:
Shannon Fernando indicated no relevant financial relationships.
Priya Sehgal indicated no relevant financial relationships.
Shannon Fernando, BA1, Priya Sehgal, MD, MS, MPH2. P3757 - Systemic Mastocytosis and the Pivotal Role of the Gastroenterologist, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
