Tuesday Poster Session
Category: Colon
P3795 - Chronic Mesenteric Ischemia With Celiac and Superior Mesenteric Arteries Occlusion in a Patient With Antiphospholipid Syndrome and Neuroendocrine Tumor: A Complex Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SS
Shahab Shayesteh, MD
Hackensack University Medical Center
Lakewood, NJ
Presenting Author(s)
Shahab Shayesteh, MD
Hackensack University Medical Center, Lakewood, NJ
Introduction: Chronic mesenteric ischemia (CMI) is a rare condition caused by reduced blood flow to the mesenteric arteries, potentially leading to bowel necrosis. It often results from atherosclerosis or thrombotic disorders and can be complicated by neuroendocrine tumors. Diagnosis involves imaging or angiography, and treatments include medication and revascularization. Early detection is vital to prevent irreversible bowel damage. This case highlights the challenges of managing CMI, antiphospholipid syndrome (APS), and neuroendocrine tumors, emphasizing prompt recognition, thorough evaluation, and a collaborative approach to effective treatment.
Case Description/Methods: A 73-year-old woman with a medical history including left ventricular thrombus, atrial fibrillation, peripheral artery disease, and previous cancer, presented with severe abdominal symptoms. Despite initial treatment, her condition worsened, revealing blockages in the celiac and superior mesenteric arteries, alongside APS. The surgery aimed to alleviate these blockages and establish alternative blood flow routes. During the aorta-superior mesenteric artery bypass surgery, a necrotic segment of the small intestine excised due to obstruction and the presence of a tumor, later identified as neuroendocrine. Following surgery, she experienced respiratory failure, anemia, and bleeding complications, leading to shock and organ failure. Despite aggressive treatment, her condition rapidly deteriorated, necessitating hospice care and eventual passing
Discussion: This case highlights the complexities in treating life-threatening CMI complications in APS and NETs patients. APS increases the risk of mesenteric artery occlusion, while NETs secrete vasoactive substances that complicate treatment. The therapeutic approach typically involves anticoagulation to prevent thrombotic events and revascularization to maintain blood flow and prevent intestinal infarction. Additionally, surgical resection or embolization of NETs is often necessary to reduce ischemia and improve patient outcomes.
This highlights the importance of continuous research to enhance management strategies and outcomes for patients with thrombotic disorders and concurrent conditions. Further research is crucial to develop the best treatments, to improve prognosis and quality of life for this vulnerable patient group.
Disclosures:
Shahab Shayesteh, MD. P3795 - Chronic Mesenteric Ischemia With Celiac and Superior Mesenteric Arteries Occlusion in a Patient With Antiphospholipid Syndrome and Neuroendocrine Tumor: A Complex Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Hackensack University Medical Center, Lakewood, NJ
Introduction: Chronic mesenteric ischemia (CMI) is a rare condition caused by reduced blood flow to the mesenteric arteries, potentially leading to bowel necrosis. It often results from atherosclerosis or thrombotic disorders and can be complicated by neuroendocrine tumors. Diagnosis involves imaging or angiography, and treatments include medication and revascularization. Early detection is vital to prevent irreversible bowel damage. This case highlights the challenges of managing CMI, antiphospholipid syndrome (APS), and neuroendocrine tumors, emphasizing prompt recognition, thorough evaluation, and a collaborative approach to effective treatment.
Case Description/Methods: A 73-year-old woman with a medical history including left ventricular thrombus, atrial fibrillation, peripheral artery disease, and previous cancer, presented with severe abdominal symptoms. Despite initial treatment, her condition worsened, revealing blockages in the celiac and superior mesenteric arteries, alongside APS. The surgery aimed to alleviate these blockages and establish alternative blood flow routes. During the aorta-superior mesenteric artery bypass surgery, a necrotic segment of the small intestine excised due to obstruction and the presence of a tumor, later identified as neuroendocrine. Following surgery, she experienced respiratory failure, anemia, and bleeding complications, leading to shock and organ failure. Despite aggressive treatment, her condition rapidly deteriorated, necessitating hospice care and eventual passing
Discussion: This case highlights the complexities in treating life-threatening CMI complications in APS and NETs patients. APS increases the risk of mesenteric artery occlusion, while NETs secrete vasoactive substances that complicate treatment. The therapeutic approach typically involves anticoagulation to prevent thrombotic events and revascularization to maintain blood flow and prevent intestinal infarction. Additionally, surgical resection or embolization of NETs is often necessary to reduce ischemia and improve patient outcomes.
This highlights the importance of continuous research to enhance management strategies and outcomes for patients with thrombotic disorders and concurrent conditions. Further research is crucial to develop the best treatments, to improve prognosis and quality of life for this vulnerable patient group.
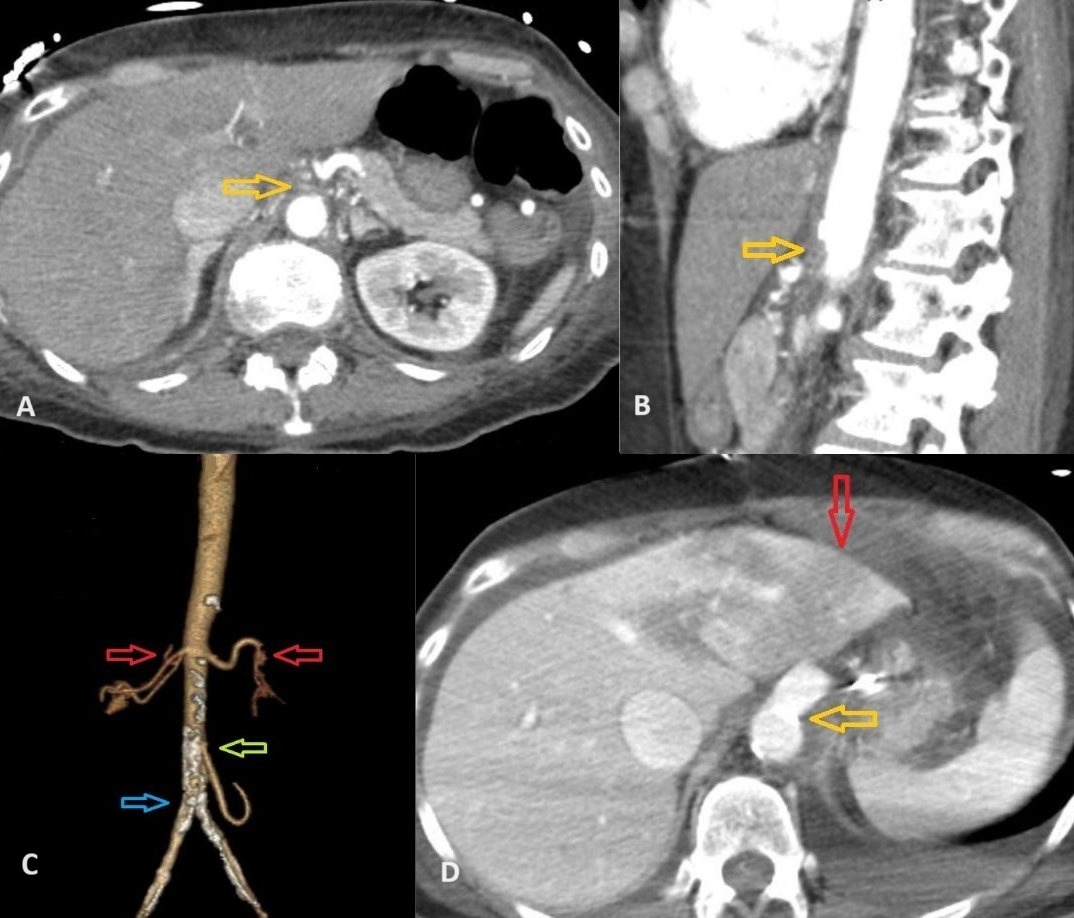
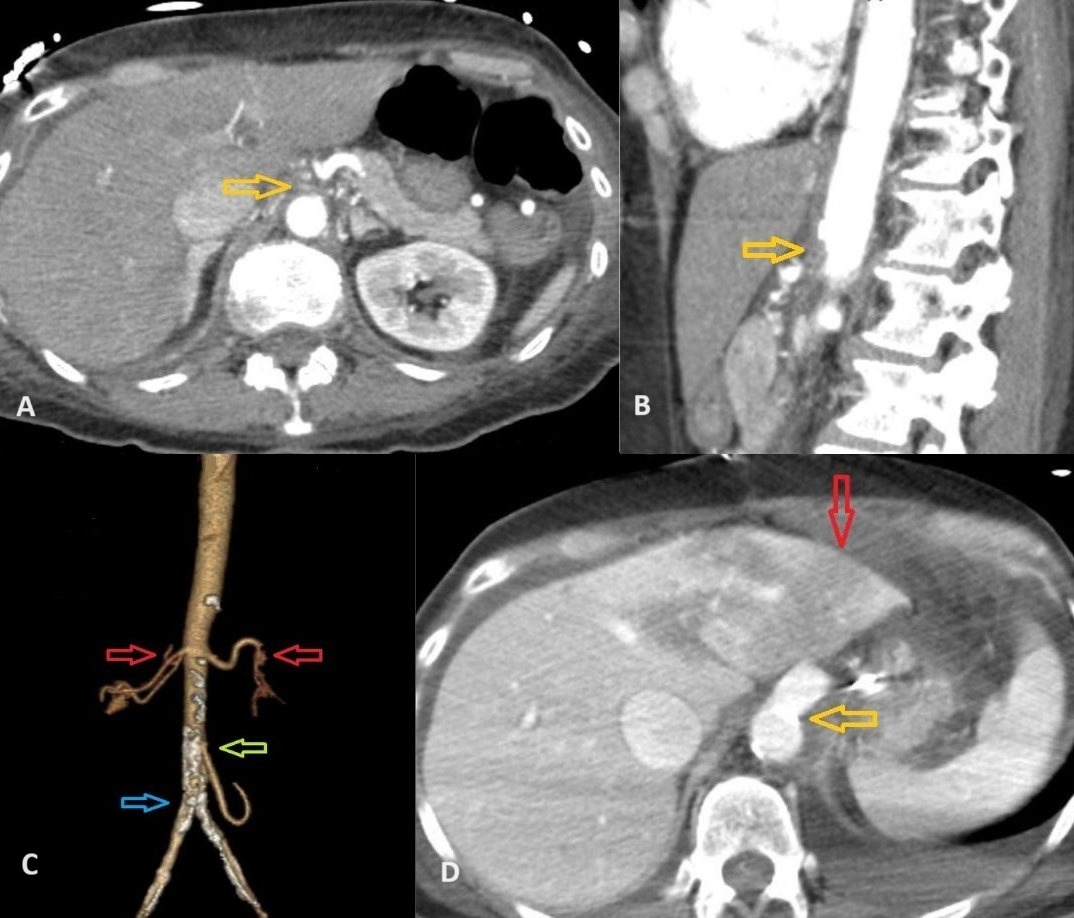
Figure: A. Yellow arrow indicating occlusions in the proximal celiac axis.
B. Yellow arrow highlighting the occlusion in the superior mesenteric artery.
C. Red arrows indicating renal arteries; green arrow pointing to the branching inferior mesenteric artery; blue arrow marking the bifurcation of the abdominal aorta. The celiac artery and superior mesenteric artery are not visible due to occlusion.
D. Post-bypass, resolved occlusion in the superior mesenteric artery indicated by the yellow arrow. The red arrow shows left lobe liver hypoattenuation consistent with ischemic hepatitis.
B. Yellow arrow highlighting the occlusion in the superior mesenteric artery.
C. Red arrows indicating renal arteries; green arrow pointing to the branching inferior mesenteric artery; blue arrow marking the bifurcation of the abdominal aorta. The celiac artery and superior mesenteric artery are not visible due to occlusion.
D. Post-bypass, resolved occlusion in the superior mesenteric artery indicated by the yellow arrow. The red arrow shows left lobe liver hypoattenuation consistent with ischemic hepatitis.
Disclosures:
Shahab Shayesteh indicated no relevant financial relationships.
Shahab Shayesteh, MD. P3795 - Chronic Mesenteric Ischemia With Celiac and Superior Mesenteric Arteries Occlusion in a Patient With Antiphospholipid Syndrome and Neuroendocrine Tumor: A Complex Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
