Tuesday Poster Session
Category: Colon
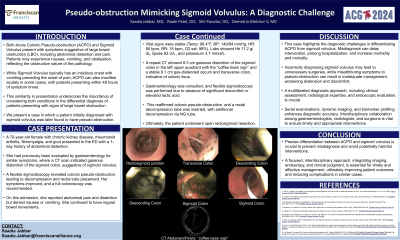
P3801 - Pseudo-Obstruction Mimicking Sigmoid Volvulus: A Diagnostic Challenge
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Saadia Jabbar, MD
Franciscan Health Olympia Fields
Homewood, IL
Presenting Author(s)
Saadia Jabbar, MD1, Raahi Patel, DO2, Shil Punatar, DO3, Melchor Demetria, MD4
1Franciscan Health Olympia Fields, Homewood, IL; 2Franciscan Health Olympia Fields, Olympia Fields, IL; 3Franciscan Health Olympia Fields, Chicago, IL; 4Franciscan Health Olympia Fields, Cook County, IL
Introduction: Acute Colonic Pseudo-Obstruction (ACPO) and Sigmoid Volvulus share similar symptoms of large bowel obstruction, such as abdominal distension, pain, nausea, vomiting, and constipation. While Sigmoid Volvulus typically presents gradually, ACPO can occur acutely, complicating the diagnosis. This report discusses a case initially misdiagnosed as sigmoid volvulus but later identified as pseudo-obstruction.
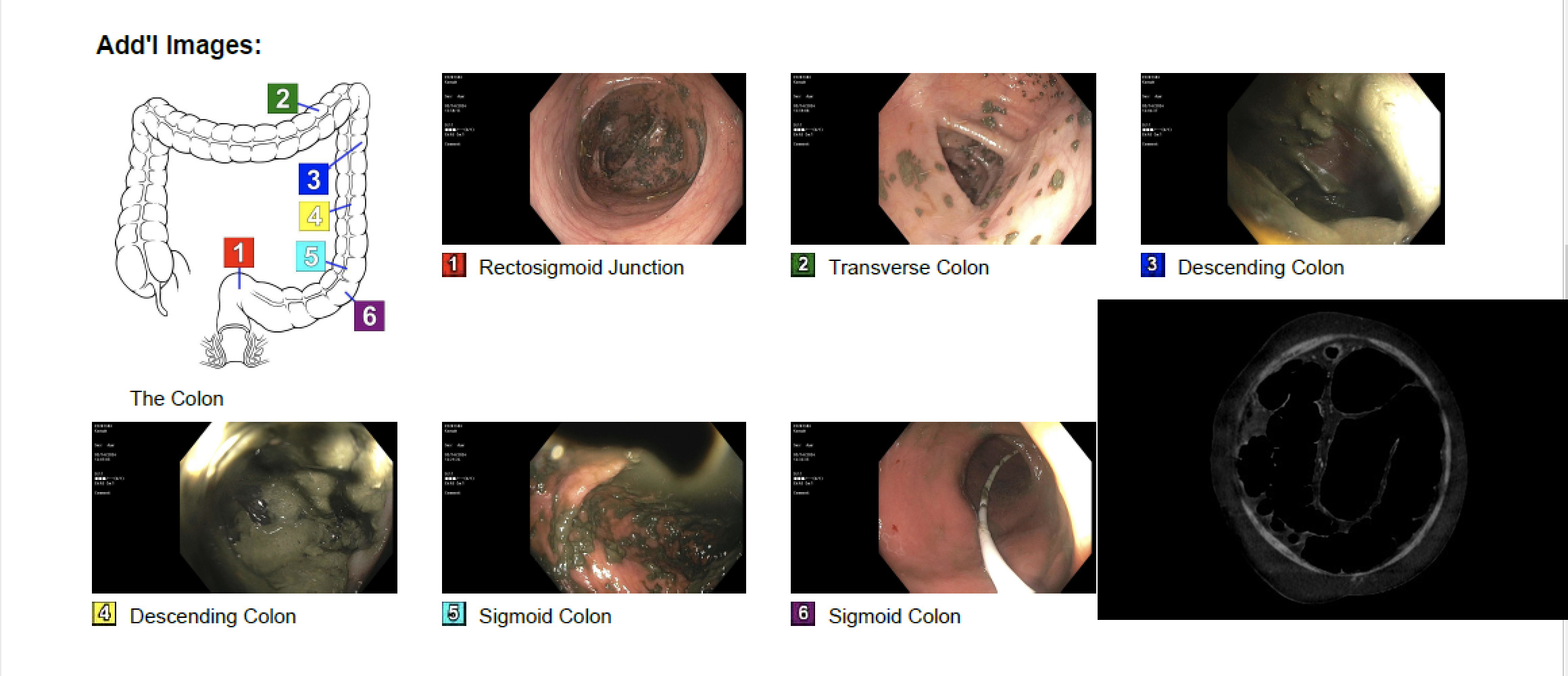
Case Description/Methods: A 70-year-old woman with chronic kidney disease and rheumatoid arthritis presented with a 1-day history of abdominal distension. She had a prior episode where a CT scan suggested sigmoid volvulus. An urgent flexible sigmoidoscopy revealed pseudo-obstruction throughout the colon, prompting decompression and rectal tube placement, which alleviated her symptoms.
During her recurrent admission, she reported severe pain and distension, avoiding food and drink without relief. However, she continued to have regular bowel movements without nausea or vomiting. Her vital signs were stable, and laboratory tests showed hemoglobin 11.2 g/dL, lipase 63 U/L, and potassium 3.7 mmol/L. A repeat CT scan again suggested sigmoid volvulus with the classic "coffee bean sign" and colonic ileus. Despite the imaging findings, flexible sigmoidoscopy reaffirmed the diagnosis of pseudo-obstruction, not volvulus, and another rectal decompression tube was placed, leading to clinical improvement. The patient eventually underwent open rectosigmoid colon resection.
Discussion: This case underscores the diagnostic challenges in differentiating ACPO from sigmoid volvulus. Misdiagnosis can delay appropriate intervention, prolong hospitalization, and increase morbidity and mortality. Incorrectly diagnosing sigmoid volvulus may lead to unnecessary surgeries, while attributing symptoms to pseudo-obstruction can result in inadequate management, worsening distension and discomfort. A comprehensive diagnostic approach, encompassing clinical assessment, radiological expertise, and endoscopic evaluation, is crucial. Serial examinations, dynamic imaging, and biomarker profiling enhance diagnostic accuracy. Interdisciplinary collaboration among gastroenterologists, radiologists, and surgeons is vital to ensure timely and appropriate interventions, ultimately improving patient outcomes in such complex cases.
Disclosures:
Saadia Jabbar, MD1, Raahi Patel, DO2, Shil Punatar, DO3, Melchor Demetria, MD4. P3801 - Pseudo-Obstruction Mimicking Sigmoid Volvulus: A Diagnostic Challenge, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Franciscan Health Olympia Fields, Homewood, IL; 2Franciscan Health Olympia Fields, Olympia Fields, IL; 3Franciscan Health Olympia Fields, Chicago, IL; 4Franciscan Health Olympia Fields, Cook County, IL
Introduction: Acute Colonic Pseudo-Obstruction (ACPO) and Sigmoid Volvulus share similar symptoms of large bowel obstruction, such as abdominal distension, pain, nausea, vomiting, and constipation. While Sigmoid Volvulus typically presents gradually, ACPO can occur acutely, complicating the diagnosis. This report discusses a case initially misdiagnosed as sigmoid volvulus but later identified as pseudo-obstruction.
Case Description/Methods: A 70-year-old woman with chronic kidney disease and rheumatoid arthritis presented with a 1-day history of abdominal distension. She had a prior episode where a CT scan suggested sigmoid volvulus. An urgent flexible sigmoidoscopy revealed pseudo-obstruction throughout the colon, prompting decompression and rectal tube placement, which alleviated her symptoms.
During her recurrent admission, she reported severe pain and distension, avoiding food and drink without relief. However, she continued to have regular bowel movements without nausea or vomiting. Her vital signs were stable, and laboratory tests showed hemoglobin 11.2 g/dL, lipase 63 U/L, and potassium 3.7 mmol/L. A repeat CT scan again suggested sigmoid volvulus with the classic "coffee bean sign" and colonic ileus. Despite the imaging findings, flexible sigmoidoscopy reaffirmed the diagnosis of pseudo-obstruction, not volvulus, and another rectal decompression tube was placed, leading to clinical improvement. The patient eventually underwent open rectosigmoid colon resection.
Discussion: This case underscores the diagnostic challenges in differentiating ACPO from sigmoid volvulus. Misdiagnosis can delay appropriate intervention, prolong hospitalization, and increase morbidity and mortality. Incorrectly diagnosing sigmoid volvulus may lead to unnecessary surgeries, while attributing symptoms to pseudo-obstruction can result in inadequate management, worsening distension and discomfort. A comprehensive diagnostic approach, encompassing clinical assessment, radiological expertise, and endoscopic evaluation, is crucial. Serial examinations, dynamic imaging, and biomarker profiling enhance diagnostic accuracy. Interdisciplinary collaboration among gastroenterologists, radiologists, and surgeons is vital to ensure timely and appropriate interventions, ultimately improving patient outcomes in such complex cases.
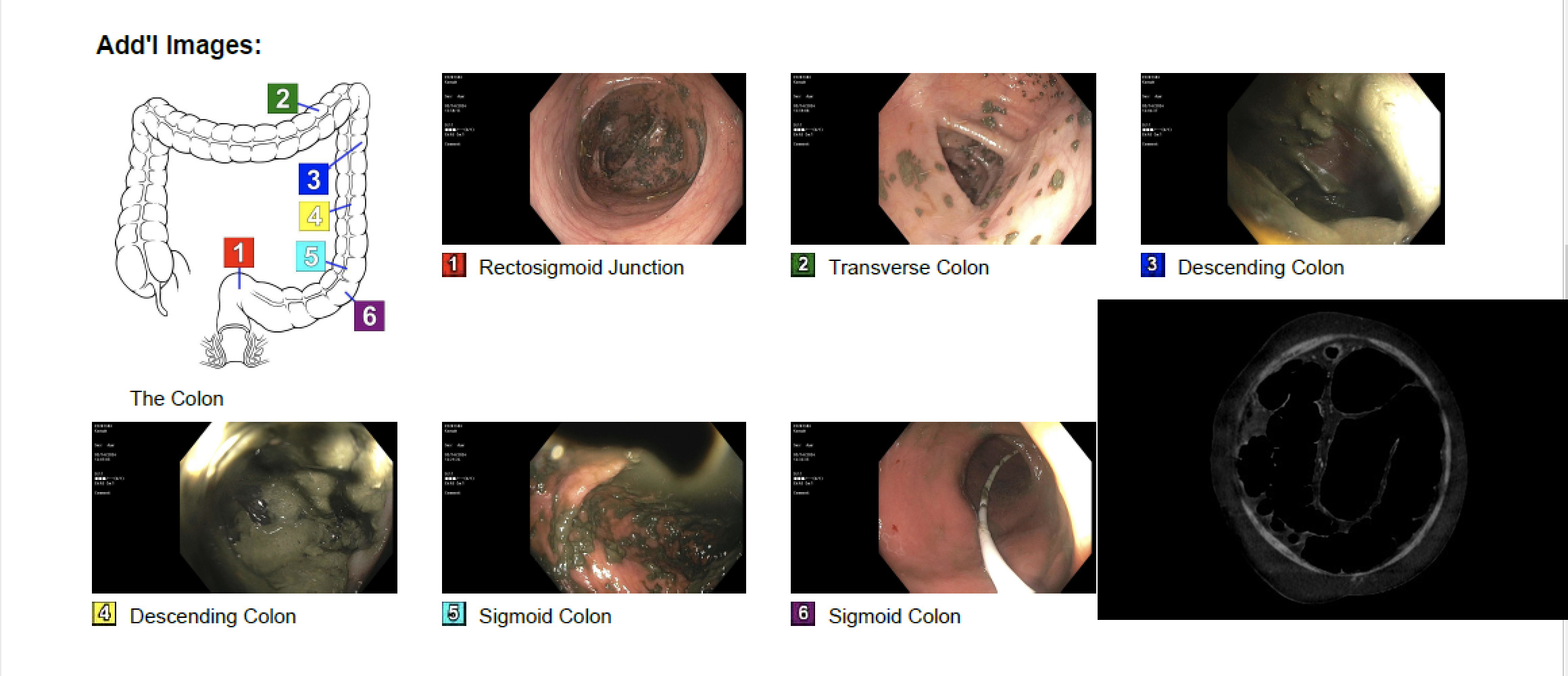
Figure: Pseudo-obstruction Mimicking Sigmoid Volvulus
Disclosures:
Saadia Jabbar indicated no relevant financial relationships.
Raahi Patel indicated no relevant financial relationships.
Shil Punatar indicated no relevant financial relationships.
Melchor Demetria indicated no relevant financial relationships.
Saadia Jabbar, MD1, Raahi Patel, DO2, Shil Punatar, DO3, Melchor Demetria, MD4. P3801 - Pseudo-Obstruction Mimicking Sigmoid Volvulus: A Diagnostic Challenge, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
