Tuesday Poster Session
Category: Colon
P3806 - Lynch Syndrome Uncovered: Identifying Anastomotic Site Recurrence Through Narrow Band Imaging
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- PS
Peter Stawinski, MD
University of Texas Health Science Center
San Antonio, TX
Presenting Author(s)
Peter Stawinski, MD1, Shuhaib Ali, DO1, Karolina N. Dziadkowiec, MD1, Andrew Han, MD2
1University of Texas Health Science Center, San Antonio, TX; 2Audie Murphy VA Hospital, San Antonio, TX
Introduction: Lynch syndrome (LS) is an autosomal dominant hereditary non-polyposis syndrome due to germline mutations in DNA mismatch repair genes resulting in microsatellite instability, accounting for 2-3% of colorectal cancers (CRC) with a mean age of diagnosis at 44-61 years. Colectomy with ileorectal anal anastomosis is the preferred treatment of LS patients affected with CRC that is unresectable by endoscopy. We present a case of a LS patient with CRC who underwent partial colectomy who later developed CRC at the ileocolonic anastomosis site (AS).
Case Description/Methods: A 60 year-old man with LS presented with symptomatic acute on chronic iron deficiency anemia with melena and 40-pound unintentional weight loss. He was diagnosed with colon adenocarcinoma (CA) at age 30 and underwent a right hemicolectomy with an end-to-end ileocolonic anastomosis followed by adjuvant chemotherapy with 5-fluorouracil. His family history pertinent for multiple paternal family members with CA. Colonoscopy (CSP) two years ago showed a patent end-to-end ileocolonic anastomosis with healthy mucosa without ulcerations. Esophagogastroduodenoscopy revealed non-bleeding erosions with gastric biopsies negative for Helicobacter pylori. CSP revealed circumferential ulcerations at the AS. Biopsies of the AS revealed poorly differentiated adenocarcinoma. Computed tomography of the chest, abdomen and pelvis showed a new enlarged retroperitoneal lymph node (LN). The patient underwent a total colectomy with end ileostomy with pathology showing poorly differentiated CA stage IIIA with a positive LN and lymphovascular invasion. He then underwent adjuvant chemotherapy.
Discussion: This is an unfortunate case of a LS patient who developed metastatic CRC after a partial colectomy for history of CRC. This case highlights the importance of appropriate counseling and surgical management for LS patients who develop CRC as the 10-year cumulative risk of CRC in patients who undergo a partial colectomy is 16-19% despite vigilant endoscopic surveillance. The differential diagnosis of anastomotic ulcers is broad to include ischemia, mechanical trauma due to motility or intussusception, medication-induced, and neoplasia, as in this case. Keeping the patient’s clinical context in mind along with a high index of suspicion was crucial to this patient’s diagnosis. Narrow band imaging is a useful tool that should be used to help identify subtle mucosal changes that can help target biopsies to cinch the diagnosis.
Disclosures:
Peter Stawinski, MD1, Shuhaib Ali, DO1, Karolina N. Dziadkowiec, MD1, Andrew Han, MD2. P3806 - Lynch Syndrome Uncovered: Identifying Anastomotic Site Recurrence Through Narrow Band Imaging, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health Science Center, San Antonio, TX; 2Audie Murphy VA Hospital, San Antonio, TX
Introduction: Lynch syndrome (LS) is an autosomal dominant hereditary non-polyposis syndrome due to germline mutations in DNA mismatch repair genes resulting in microsatellite instability, accounting for 2-3% of colorectal cancers (CRC) with a mean age of diagnosis at 44-61 years. Colectomy with ileorectal anal anastomosis is the preferred treatment of LS patients affected with CRC that is unresectable by endoscopy. We present a case of a LS patient with CRC who underwent partial colectomy who later developed CRC at the ileocolonic anastomosis site (AS).
Case Description/Methods: A 60 year-old man with LS presented with symptomatic acute on chronic iron deficiency anemia with melena and 40-pound unintentional weight loss. He was diagnosed with colon adenocarcinoma (CA) at age 30 and underwent a right hemicolectomy with an end-to-end ileocolonic anastomosis followed by adjuvant chemotherapy with 5-fluorouracil. His family history pertinent for multiple paternal family members with CA. Colonoscopy (CSP) two years ago showed a patent end-to-end ileocolonic anastomosis with healthy mucosa without ulcerations. Esophagogastroduodenoscopy revealed non-bleeding erosions with gastric biopsies negative for Helicobacter pylori. CSP revealed circumferential ulcerations at the AS. Biopsies of the AS revealed poorly differentiated adenocarcinoma. Computed tomography of the chest, abdomen and pelvis showed a new enlarged retroperitoneal lymph node (LN). The patient underwent a total colectomy with end ileostomy with pathology showing poorly differentiated CA stage IIIA with a positive LN and lymphovascular invasion. He then underwent adjuvant chemotherapy.
Discussion: This is an unfortunate case of a LS patient who developed metastatic CRC after a partial colectomy for history of CRC. This case highlights the importance of appropriate counseling and surgical management for LS patients who develop CRC as the 10-year cumulative risk of CRC in patients who undergo a partial colectomy is 16-19% despite vigilant endoscopic surveillance. The differential diagnosis of anastomotic ulcers is broad to include ischemia, mechanical trauma due to motility or intussusception, medication-induced, and neoplasia, as in this case. Keeping the patient’s clinical context in mind along with a high index of suspicion was crucial to this patient’s diagnosis. Narrow band imaging is a useful tool that should be used to help identify subtle mucosal changes that can help target biopsies to cinch the diagnosis.
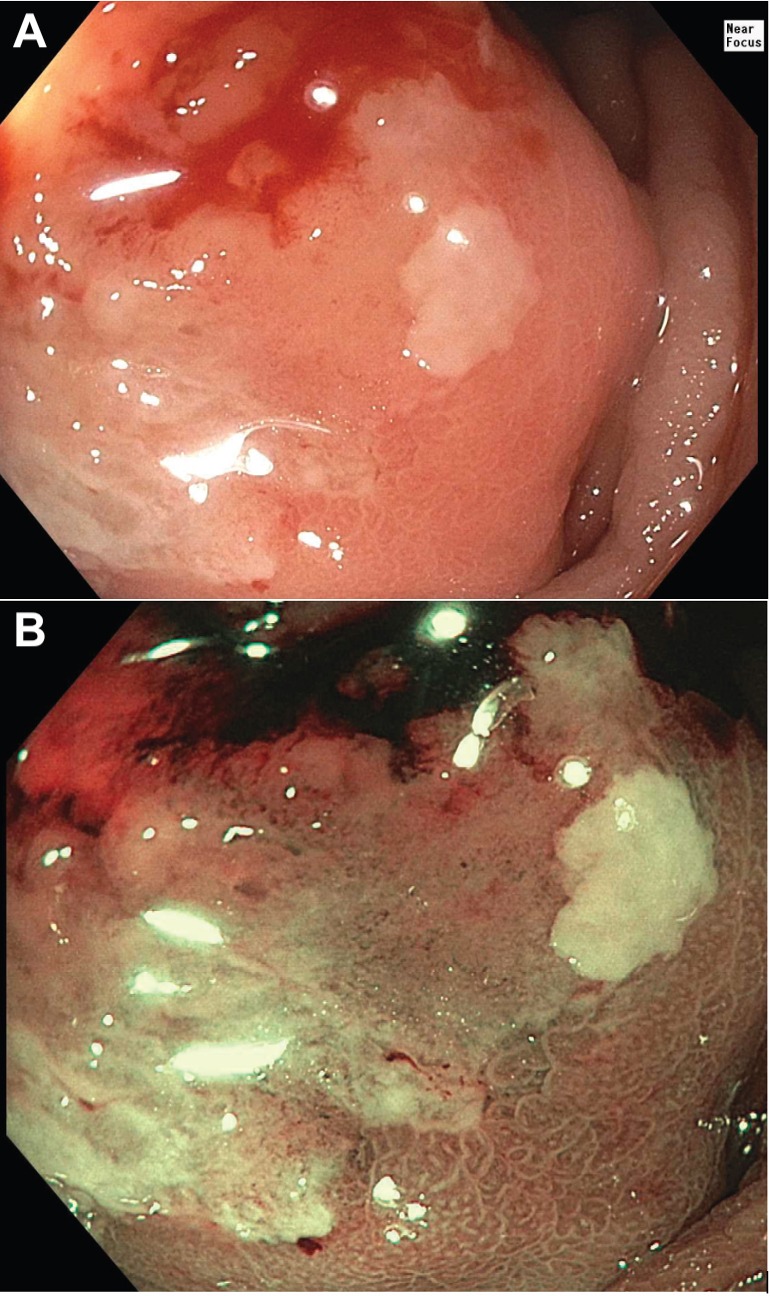
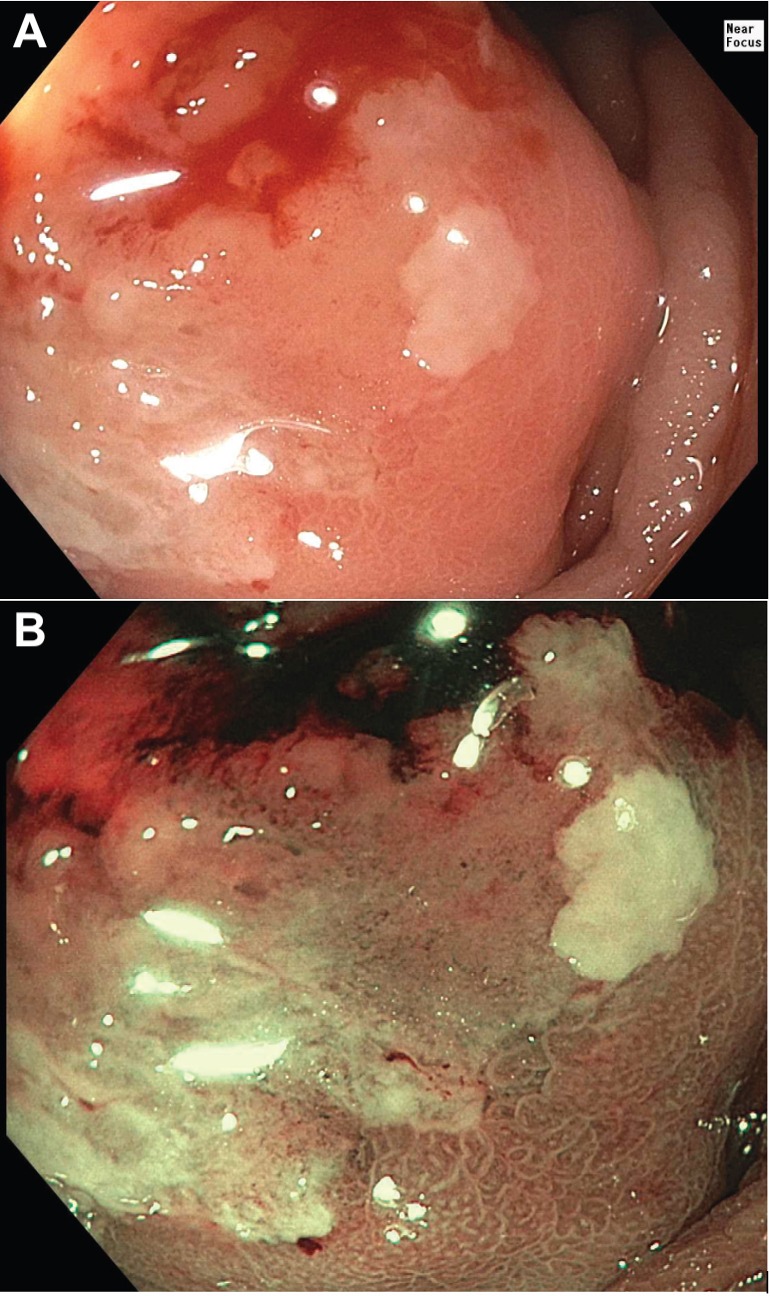
Figure: A. Magnified image showing a portion of the anastomosis under white light.
B. Magnified image captured under Narrow Band Imaging (NBI), highlighting architectural changes at the anastomosis site.
B. Magnified image captured under Narrow Band Imaging (NBI), highlighting architectural changes at the anastomosis site.
Disclosures:
Peter Stawinski indicated no relevant financial relationships.
Shuhaib Ali indicated no relevant financial relationships.
Karolina Dziadkowiec indicated no relevant financial relationships.
Andrew Han indicated no relevant financial relationships.
Peter Stawinski, MD1, Shuhaib Ali, DO1, Karolina N. Dziadkowiec, MD1, Andrew Han, MD2. P3806 - Lynch Syndrome Uncovered: Identifying Anastomotic Site Recurrence Through Narrow Band Imaging, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
