Tuesday Poster Session
Category: Colorectal Cancer Prevention
P3820 - The Impact of the COVID-19 Pandemic on an Established Hereditary Colon Cancer Registry
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SA
Srishty M. Agarwal, MBBS
Government Medical College and Hospital
Surat, Gujarat, India
Presenting Author(s)
Srishty M. Agarwal, MBBS1, Zachariah Foda, MD, PhD2, Linda Hylind, BS, RN2
1Government Medical College and Hospital, Surat, Gujarat, India; 2Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: While most cancers, including colorectal cancer (CRC) are sporadic in nature, it is estimated that at least 15% of all CRC is familial. A smaller subset is caused by monogenic mutations that lead to hereditary cancer syndromes that confer up to 100% lifetime risk of CRC, such as Lynch Syndrome (LS), and Familial adenomatous Polyposis (FAP). Due to the rarity of these conditions, registries have been crucial in our understanding of these syndromes. The purpose of this retrospective study is to investigate the impact of the clinical practice changes induced by the COVID-19 pandemic on one such registry that has enrolled patients for over 50 years.
Methods: A total of 249 patients were enrolled in the hereditary colorectal cancer registry at an academic tertiary care center between 2017 to 2023. Patient data, including age, demographics, follow-up history, medical history, genetic testing, and family history, were collected from chart reviews and surveys. Descriptive statistics were performed to compare individuals enrolled before 2020 and those after, as well as across risk factors. The student t-test was to compare patient characteristics.
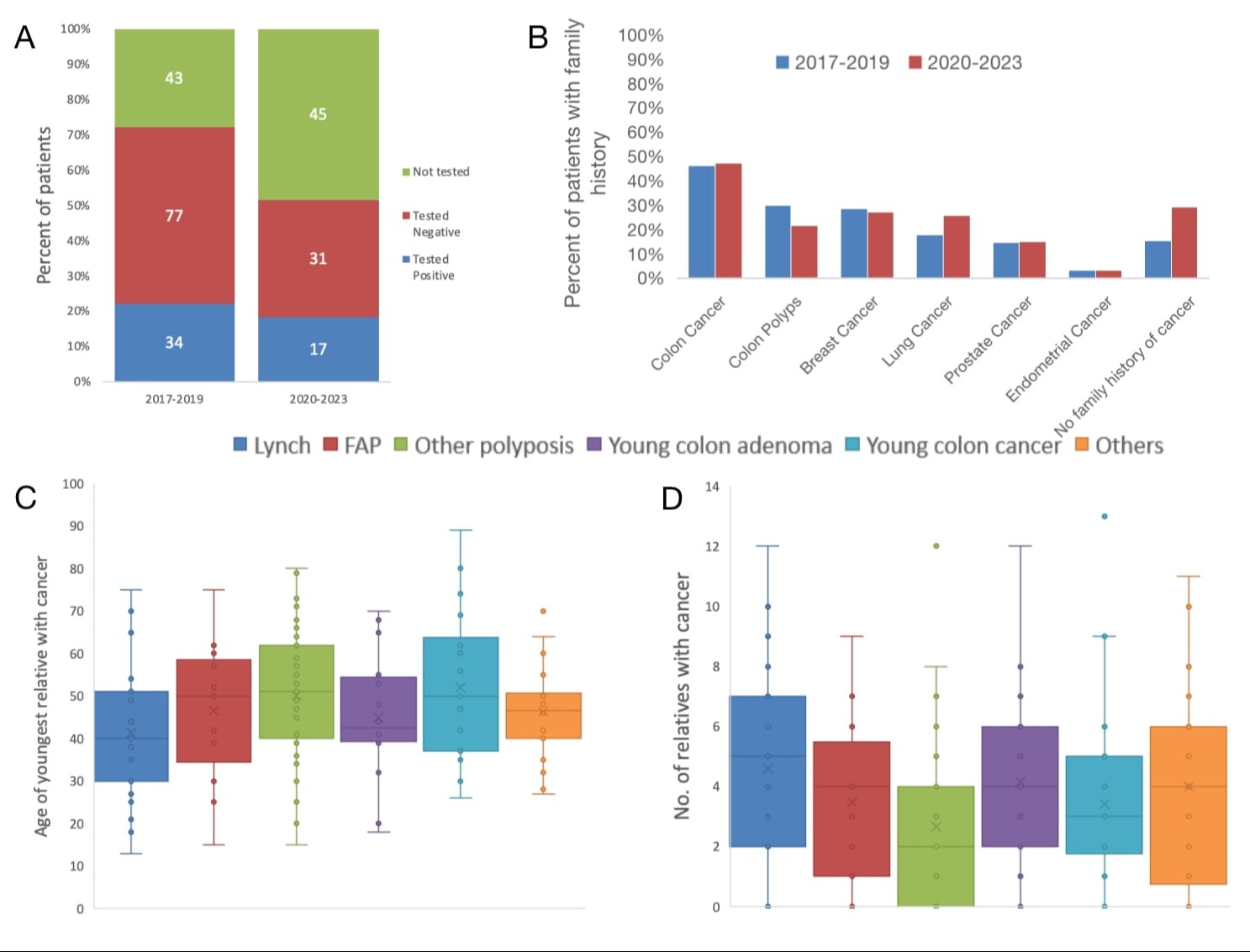
Results: Of the 249 patients, a majority of the participants were female (58%). (Table 1). The mean age in group A (2017-2019) and in group B (2020-2023) were similar (46.4 vs. 49.8 (p= 0.14)). Throughout the whole time frame, 161 patients (64.65%) underwent genetic testing of which 40% were found to have at least one pathogenic or likely pathogenic variation. Testing rates dropped from 72.4% in Group A to 51.6% in group B, although this was not statistically significant. Positivity rates were comparable over the two-time frames (21.7% vs. 18.2% p=0.8)(Figure-1A.) The mean number of genes that were tested increased from 11.61 to 16.54 (p=0.02). There was a high percentage of individuals with a family history of cancer (79%). The age of onset of cancer in those family members was earlier as compared to population averages (Figure 1B-D).
Discussion: This work examined the demographics and genetic testing of individuals enrolled in a hereditary colon cancer registry in the period before and after the COVID-19 health emergency. Other than an increase in the number of genes tested, no significant changes were identified between these periods. Follow-up was too short to identify clinical outcomes such as cancer incidence, but these could become apparent as this group of patients will continue to be followed through this registry.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Srishty M. Agarwal, MBBS1, Zachariah Foda, MD, PhD2, Linda Hylind, BS, RN2. P3820 - The Impact of the COVID-19 Pandemic on an Established Hereditary Colon Cancer Registry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Government Medical College and Hospital, Surat, Gujarat, India; 2Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: While most cancers, including colorectal cancer (CRC) are sporadic in nature, it is estimated that at least 15% of all CRC is familial. A smaller subset is caused by monogenic mutations that lead to hereditary cancer syndromes that confer up to 100% lifetime risk of CRC, such as Lynch Syndrome (LS), and Familial adenomatous Polyposis (FAP). Due to the rarity of these conditions, registries have been crucial in our understanding of these syndromes. The purpose of this retrospective study is to investigate the impact of the clinical practice changes induced by the COVID-19 pandemic on one such registry that has enrolled patients for over 50 years.
Methods: A total of 249 patients were enrolled in the hereditary colorectal cancer registry at an academic tertiary care center between 2017 to 2023. Patient data, including age, demographics, follow-up history, medical history, genetic testing, and family history, were collected from chart reviews and surveys. Descriptive statistics were performed to compare individuals enrolled before 2020 and those after, as well as across risk factors. The student t-test was to compare patient characteristics.
Results: Of the 249 patients, a majority of the participants were female (58%). (Table 1). The mean age in group A (2017-2019) and in group B (2020-2023) were similar (46.4 vs. 49.8 (p= 0.14)). Throughout the whole time frame, 161 patients (64.65%) underwent genetic testing of which 40% were found to have at least one pathogenic or likely pathogenic variation. Testing rates dropped from 72.4% in Group A to 51.6% in group B, although this was not statistically significant. Positivity rates were comparable over the two-time frames (21.7% vs. 18.2% p=0.8)(Figure-1A.) The mean number of genes that were tested increased from 11.61 to 16.54 (p=0.02). There was a high percentage of individuals with a family history of cancer (79%). The age of onset of cancer in those family members was earlier as compared to population averages (Figure 1B-D).
Discussion: This work examined the demographics and genetic testing of individuals enrolled in a hereditary colon cancer registry in the period before and after the COVID-19 health emergency. Other than an increase in the number of genes tested, no significant changes were identified between these periods. Follow-up was too short to identify clinical outcomes such as cancer incidence, but these could become apparent as this group of patients will continue to be followed through this registry.
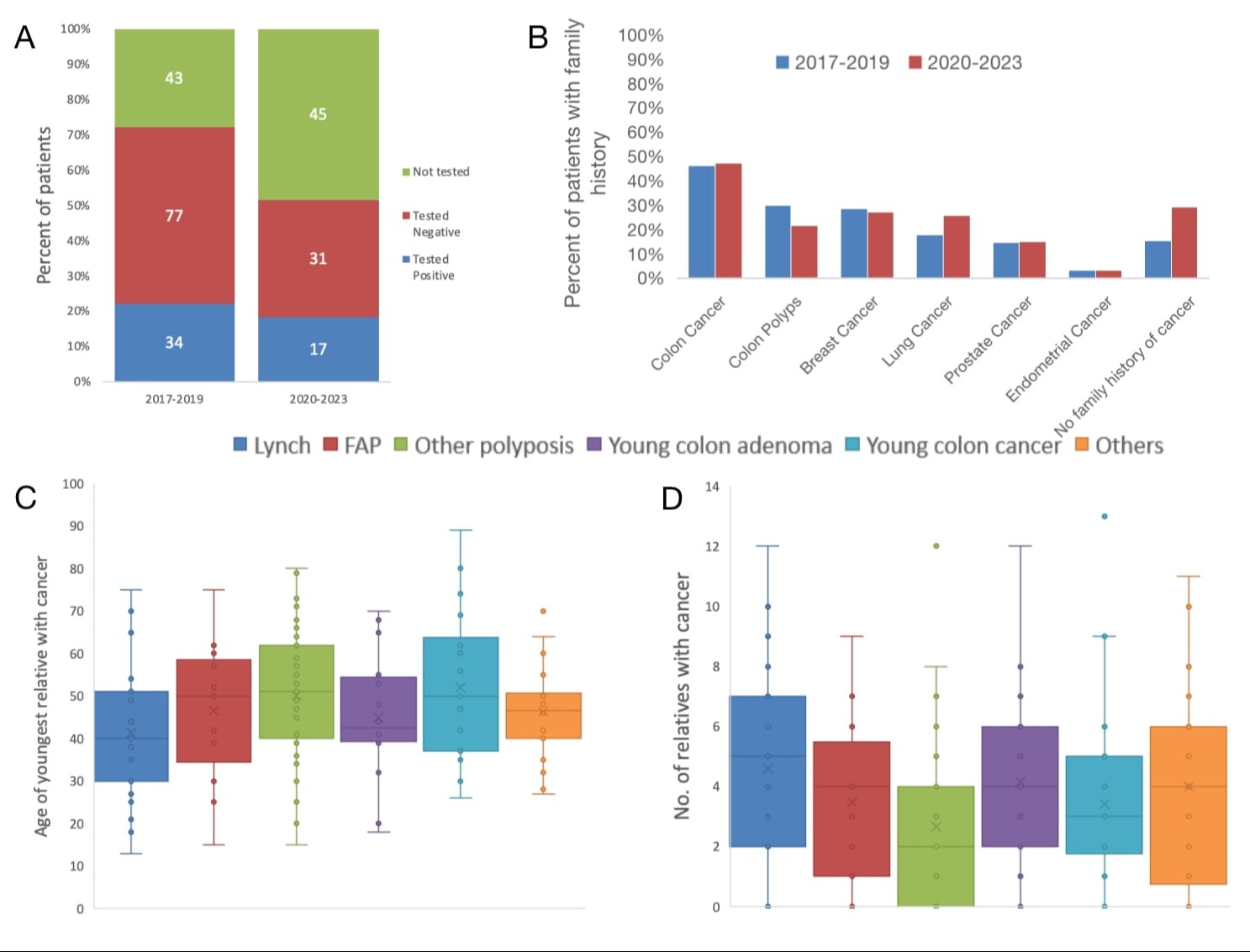
Figure: Figure 1: Family history and Genetic testing practice did not differ between study periods. A- Genetic testing and positivity rates were similar between time periods. All patient groups are represented, and data labels represent the number of patients in each group. B High prevalence of family history of colonic and extracolonic cancers was similar between time periods. C-D Multiple family members had cancer, and the average age of onset was young. Data represents each cancer syndrome throughout the whole study.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Srishty Agarwal indicated no relevant financial relationships.
Zachariah Foda: Delfi Diagnostics – Intellectual Property/Patents, Royalties.
Linda Hylind indicated no relevant financial relationships.
Srishty M. Agarwal, MBBS1, Zachariah Foda, MD, PhD2, Linda Hylind, BS, RN2. P3820 - The Impact of the COVID-19 Pandemic on an Established Hereditary Colon Cancer Registry, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
