Tuesday Poster Session
Category: Esophagus
P3900 - Identifying the Prevalence of Barrett’s Esophagus and Esophageal Adenocarcinoma Screening Rates Based on the 2022 AGA Screening Guidelines in a Population Undergoing Screening Colonoscopies
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jaya Chandra, MD
Mercy Health St. Rita's Medical Center
Lima, OH
Presenting Author(s)
Jaya Chandra, MD, Jayde E.. Kurland, MD, FACG
Mercy Health St. Rita's Medical Center, Lima, OH
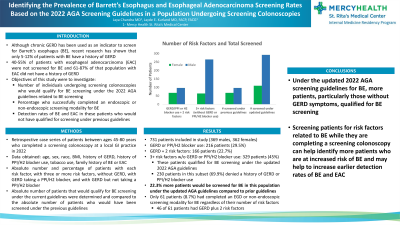
Introduction: This research study sought to investigate the number of individuals undergoing screening colonoscopies who would qualify for Barrett’s Esophagus (BE) screening under the 2022 American Gastroenterological Association guidelines related to BE screening, the percentage who successfully completed an endoscopic or non-endoscopic screening modality for BE, and the detection rates of BE and esophageal adenocarcinoma (EAC) in these patients who would not have qualified for screening under the previous guidelines.
Methods: Patients aged 45 to 80 years who completed a screening colonoscopy at a local gastroenterology practice in 2022 were included in this retrospective study. Demographic information collected included age, sex, race, BMI, history of GERD, history of proton pump inhibitor or H2 blocker use, tobacco use, family history of BE or EAC. EGD results were collected for patients if they had an EGD after they had completed the screening colonoscopy.
Results: Of the 731 patients included (369 males, 362 females), 216 patients (29.5% of sample population) reported a history of GERD or PPI/H2 blocker use, 166 patients (22.7% of sample population) had a history of GERD and two additional risk factors for BE, and 329 patients (45.0% of sample population) had three or more risk factors for BE without GERD or PPI/H2 blocker use as a risk factor. Of the 329 patients who qualified for screening under the new guidelines, 230 patients denied a history of GERD or PPI/H2 blocker use (69.9% of this subset of patients). Based on the results obtained with this population, 22.3% more patients would be screened for BE under the updated AGA guidelines. In the sample population, only 61 patients (8.7% of sample population) had completed an EGD or non-endoscopic screening modality for BE regardless of their number of risk factors and 46 of 61 patients had GERD plus two additional risk factors.
Discussion: These results demonstrate that there may be a benefit in evaluating patients for risk factors related to BE while they are at their visit to complete their screening colonoscopies. Since there are several patients who undergo screening colonoscopies without a prior outpatient visit with a GI provider to assess for risk factors for other GI-related conditions such as BE, screening patients for risk factors related to BE while they are completing a screening colonoscopy may help identify more patients who are at increased risk of BE and may help to increase earlier detection rates of BE and EAC.
Disclosures:
Jaya Chandra, MD, Jayde E.. Kurland, MD, FACG. P3900 - Identifying the Prevalence of Barrett’s Esophagus and Esophageal Adenocarcinoma Screening Rates Based on the 2022 AGA Screening Guidelines in a Population Undergoing Screening Colonoscopies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mercy Health St. Rita's Medical Center, Lima, OH
Introduction: This research study sought to investigate the number of individuals undergoing screening colonoscopies who would qualify for Barrett’s Esophagus (BE) screening under the 2022 American Gastroenterological Association guidelines related to BE screening, the percentage who successfully completed an endoscopic or non-endoscopic screening modality for BE, and the detection rates of BE and esophageal adenocarcinoma (EAC) in these patients who would not have qualified for screening under the previous guidelines.
Methods: Patients aged 45 to 80 years who completed a screening colonoscopy at a local gastroenterology practice in 2022 were included in this retrospective study. Demographic information collected included age, sex, race, BMI, history of GERD, history of proton pump inhibitor or H2 blocker use, tobacco use, family history of BE or EAC. EGD results were collected for patients if they had an EGD after they had completed the screening colonoscopy.
Results: Of the 731 patients included (369 males, 362 females), 216 patients (29.5% of sample population) reported a history of GERD or PPI/H2 blocker use, 166 patients (22.7% of sample population) had a history of GERD and two additional risk factors for BE, and 329 patients (45.0% of sample population) had three or more risk factors for BE without GERD or PPI/H2 blocker use as a risk factor. Of the 329 patients who qualified for screening under the new guidelines, 230 patients denied a history of GERD or PPI/H2 blocker use (69.9% of this subset of patients). Based on the results obtained with this population, 22.3% more patients would be screened for BE under the updated AGA guidelines. In the sample population, only 61 patients (8.7% of sample population) had completed an EGD or non-endoscopic screening modality for BE regardless of their number of risk factors and 46 of 61 patients had GERD plus two additional risk factors.
Discussion: These results demonstrate that there may be a benefit in evaluating patients for risk factors related to BE while they are at their visit to complete their screening colonoscopies. Since there are several patients who undergo screening colonoscopies without a prior outpatient visit with a GI provider to assess for risk factors for other GI-related conditions such as BE, screening patients for risk factors related to BE while they are completing a screening colonoscopy may help identify more patients who are at increased risk of BE and may help to increase earlier detection rates of BE and EAC.
Disclosures:
Jaya Chandra indicated no relevant financial relationships.
Jayde Kurland indicated no relevant financial relationships.
Jaya Chandra, MD, Jayde E.. Kurland, MD, FACG. P3900 - Identifying the Prevalence of Barrett’s Esophagus and Esophageal Adenocarcinoma Screening Rates Based on the 2022 AGA Screening Guidelines in a Population Undergoing Screening Colonoscopies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
