Tuesday Poster Session
Category: Esophagus
P3902 - Functional Luminal Imaging Probe (FLIP) Parameters Can Be Used to Classify Cause of Treatment Failure in Achalasia
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Alam Merchant, MD
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Alam Merchant, MD1, William Breaux, MD1, Seth Force, MD1, Steven Keilin, MD1, Edward Lin, DO, MBA2, Scott Davis, MD1, Felix G. Fernandez, MD3, Anand Jain, MD4
1Emory University School of Medicine, Atlanta, GA; 2Emory University School of Medicine, Decatur, GA; 3Emory Clinic/Emory Healthcare, Atlanta, GA; 4Emory University, Atlanta, GA
Introduction: Causes of myotomy failure in achalasia are variable and can be difficult to discern. Recent studies have shown that functional lumen imaging probe (FLIP) panometry is accurate in diagnosing esophagogastric junction (EGJ) obstruction after myotomy in achalasia. In this study, we examined whether FLIP can differentiate the specific cause of EGJ obstruction in cases of recurrent symptoms after myotomy.
Methods: We performed a retrospective analysis of adult subjects referred to the Esophageal Clinic at our institution for indication of recurrent dysphagia after definitive achalasia therapy [laparoscopic Heller myotomy (LHM), per-oral endoscopic myotomy (POEM), or pneumatic dilation (PD)]. All subjects whom underwent esophagogastroduodenoscopy (EGD) with FLIP, high-resolution manometry (HRM), and barium esophagram were included. Data from these procedures were utilized to classify treatment failure causes by a multidisciplinary panel comprised of experienced gastroenterologists, cardiothoracic surgeons, and gastrointestinal surgeons as i) recurrent LES dysfunction, ii) EGJ obstruction which could be from the fundoplication or LES, iii) esophageal body dilatation/deformity, iv) peptic or other stricture, v), spastic muscular segment in esophageal body, or vi) not enough information/none of the above. One way ANOVA and unpaired two-sided t-test were used for analyses.
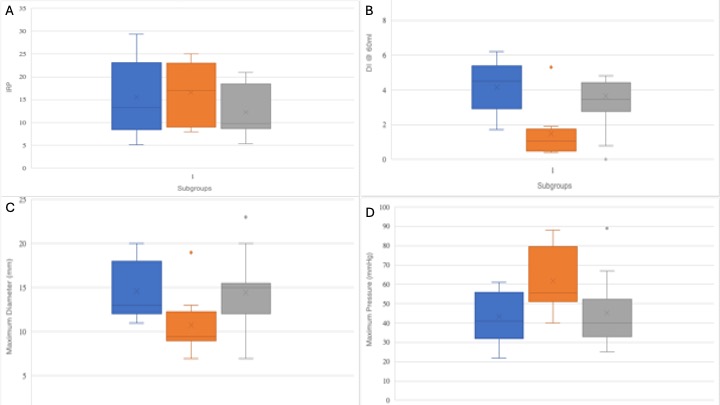
Results: Forty-two patients were included. Clinical data for the sample are shown in Table 1. The most common causes of recurrent symptoms were esophageal body dilation/deformity, followed by EGJ obstruction and recurrent LES dysfunction. EGJ opening in the setting of LES dysfunction was most impaired as measured by the DI (1.5 ± 1.6, vs 4.2 ± 1.5 in EGJ obstruction, vs 3.9 ± 2.1 in dilation/deformity, one-way ANOVA p = 0.007), max EGJ diameter (10.8mm ± 3.7, vs 14.6mm ± 3.3 in EGJ obstruction, vs 14.5mm ± 3.9 in dilation/deformity, one-way ANOVA p = .055), and maximal pressure (61.9 mmHg ± 16.9, vs 43.4 mmHg ± 12.9 in EGJ obstruction, vs 45.3 mmHg ± 17.1 in dilation/deformity, one-way ANOVA p = 0.04) (Figure 1).
Discussion: EGJ opening measures on FLIP are effective at differentiating achalasia treatment failures due to EGJ obstruction vs anatomic changes. An EGJ-DI of < 1 likely indicates recurrent LES dysfunction and may be useful in selecting patients to undergo additional myotomy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alam Merchant, MD1, William Breaux, MD1, Seth Force, MD1, Steven Keilin, MD1, Edward Lin, DO, MBA2, Scott Davis, MD1, Felix G. Fernandez, MD3, Anand Jain, MD4. P3902 - Functional Luminal Imaging Probe (FLIP) Parameters Can Be Used to Classify Cause of Treatment Failure in Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Emory University School of Medicine, Atlanta, GA; 2Emory University School of Medicine, Decatur, GA; 3Emory Clinic/Emory Healthcare, Atlanta, GA; 4Emory University, Atlanta, GA
Introduction: Causes of myotomy failure in achalasia are variable and can be difficult to discern. Recent studies have shown that functional lumen imaging probe (FLIP) panometry is accurate in diagnosing esophagogastric junction (EGJ) obstruction after myotomy in achalasia. In this study, we examined whether FLIP can differentiate the specific cause of EGJ obstruction in cases of recurrent symptoms after myotomy.
Methods: We performed a retrospective analysis of adult subjects referred to the Esophageal Clinic at our institution for indication of recurrent dysphagia after definitive achalasia therapy [laparoscopic Heller myotomy (LHM), per-oral endoscopic myotomy (POEM), or pneumatic dilation (PD)]. All subjects whom underwent esophagogastroduodenoscopy (EGD) with FLIP, high-resolution manometry (HRM), and barium esophagram were included. Data from these procedures were utilized to classify treatment failure causes by a multidisciplinary panel comprised of experienced gastroenterologists, cardiothoracic surgeons, and gastrointestinal surgeons as i) recurrent LES dysfunction, ii) EGJ obstruction which could be from the fundoplication or LES, iii) esophageal body dilatation/deformity, iv) peptic or other stricture, v), spastic muscular segment in esophageal body, or vi) not enough information/none of the above. One way ANOVA and unpaired two-sided t-test were used for analyses.
Results: Forty-two patients were included. Clinical data for the sample are shown in Table 1. The most common causes of recurrent symptoms were esophageal body dilation/deformity, followed by EGJ obstruction and recurrent LES dysfunction. EGJ opening in the setting of LES dysfunction was most impaired as measured by the DI (1.5 ± 1.6, vs 4.2 ± 1.5 in EGJ obstruction, vs 3.9 ± 2.1 in dilation/deformity, one-way ANOVA p = 0.007), max EGJ diameter (10.8mm ± 3.7, vs 14.6mm ± 3.3 in EGJ obstruction, vs 14.5mm ± 3.9 in dilation/deformity, one-way ANOVA p = .055), and maximal pressure (61.9 mmHg ± 16.9, vs 43.4 mmHg ± 12.9 in EGJ obstruction, vs 45.3 mmHg ± 17.1 in dilation/deformity, one-way ANOVA p = 0.04) (Figure 1).
Discussion: EGJ opening measures on FLIP are effective at differentiating achalasia treatment failures due to EGJ obstruction vs anatomic changes. An EGJ-DI of < 1 likely indicates recurrent LES dysfunction and may be useful in selecting patients to undergo additional myotomy.
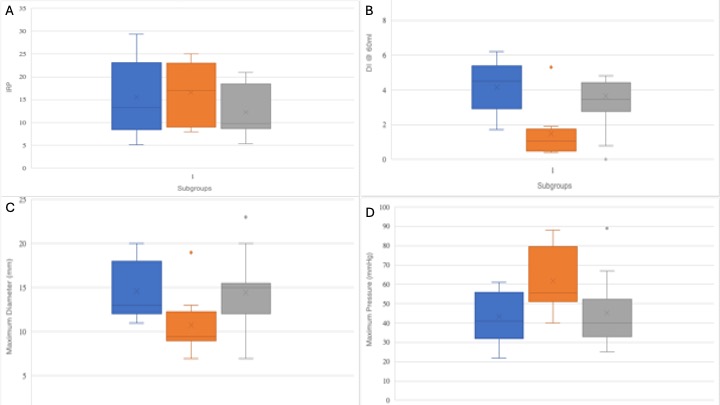
Figure: Figure 1A: Integrated Relaxation Pressure (IRP) in Treatment Failure Subgroups. Blue = EGJ Obstruction. Orange = Recurrent LES Dysfunction. Gray = Dilation/Deformity. EGJ Obstruction vs Recurrent LES, p = 0.78. Recurrent LES vs Dilation/Deformity, p = 0.16. Dilation/Deformity vs EGJ Obstruction, p = 0.29 One-way ANOVA, p = 0.38.
Figure 1B: Distensibility Index (DI) in Treatment Failure Subgroups. Blue = EGJ Obstruction. Orange = Recurrent LES Dysfunction. Gray = Dilation/Deformity. EGJ Obstruction vs Recurrent LES, p = 0.002. Recurrent LES vs Dilation/Deformity, p = 0.01. Dilation/Deformity vs EGJ Obstruction, p = 0.78. One-way ANOVA, p = 0.007
Figure 1C: Maximum Diameter in Treatment Failure Subgroups. Blue = EGJ Obstruction. Orange = Recurrent LES Dysfunction. Gray = Dilation/Deformity. EGJ Obstruction vs Recurrent LES, p = 0.03. Recurrent LES vs Dilation/Deformity, p = 0.05. Dilation/Deformity vs EGJ Obstruction, p = 0.9. One-way ANOVA, p = 0.055
Figure 1D: Maximum Pressure in Treatment Failure Subgroups. Blue = EGJ Obstruction. Orange = Recurrent LES Dysfunction. Gray = Dilation/Deformity. EGJ Obstruction vs Recurrent LES, p = 0.01. Recurrent LES vs Dilation/Deformity, p = 0.04. Dilation/Deformity vs EGJ Obstruction, p = 0.76. One-way ANOVA, p = 0.036.
Figure 1B: Distensibility Index (DI) in Treatment Failure Subgroups. Blue = EGJ Obstruction. Orange = Recurrent LES Dysfunction. Gray = Dilation/Deformity. EGJ Obstruction vs Recurrent LES, p = 0.002. Recurrent LES vs Dilation/Deformity, p = 0.01. Dilation/Deformity vs EGJ Obstruction, p = 0.78. One-way ANOVA, p = 0.007
Figure 1C: Maximum Diameter in Treatment Failure Subgroups. Blue = EGJ Obstruction. Orange = Recurrent LES Dysfunction. Gray = Dilation/Deformity. EGJ Obstruction vs Recurrent LES, p = 0.03. Recurrent LES vs Dilation/Deformity, p = 0.05. Dilation/Deformity vs EGJ Obstruction, p = 0.9. One-way ANOVA, p = 0.055
Figure 1D: Maximum Pressure in Treatment Failure Subgroups. Blue = EGJ Obstruction. Orange = Recurrent LES Dysfunction. Gray = Dilation/Deformity. EGJ Obstruction vs Recurrent LES, p = 0.01. Recurrent LES vs Dilation/Deformity, p = 0.04. Dilation/Deformity vs EGJ Obstruction, p = 0.76. One-way ANOVA, p = 0.036.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alam Merchant indicated no relevant financial relationships.
William Breaux indicated no relevant financial relationships.
Seth Force indicated no relevant financial relationships.
Steven Keilin indicated no relevant financial relationships.
Edward Lin indicated no relevant financial relationships.
Scott Davis: Intuitive surgical – Surgical proctor.
Felix Fernandez indicated no relevant financial relationships.
Anand Jain indicated no relevant financial relationships.
Alam Merchant, MD1, William Breaux, MD1, Seth Force, MD1, Steven Keilin, MD1, Edward Lin, DO, MBA2, Scott Davis, MD1, Felix G. Fernandez, MD3, Anand Jain, MD4. P3902 - Functional Luminal Imaging Probe (FLIP) Parameters Can Be Used to Classify Cause of Treatment Failure in Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
