Tuesday Poster Session
Category: Esophagus
P3903 - Identifying Predictors of On-Time Surveillance in Patients With Barrett’s Esophagus Post-Endoscopic Eradication Therapy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- PC
Paras Singh Chandi, MBBS
Mayo Clinic
Rochester, MN
Presenting Author(s)
Paras Singh Chandi, MBBS1, Fangfang Wang, MD2, Sean Sileno, MD3, Han Zhang, MD4, Anjul Verma, MD1, Laura E. Bach, DO5, Prasad G. Iyer, MD, MS, FACG3, Allon Kahn, MD6
1Mayo Clinic, Rochester, MN; 2Mayo Clinic Arizona, Scottsdale, AZ; 3Mayo Clinic, Phoenix, AZ; 4Scripps Clinic, La Jolla, CA; 5Mayo Clinic College of Medicine and Science, Oro Valley, AZ; 6Mayo Clinic, Scottsdale, AZ
Introduction: Current Barrett’s esophagus (BE) guidelines recommend endoscopic surveillance after complete eradication of intestinal metaplasia (CE-IM) at intervals determined by pre-treatment histology. We have previously reported unexpectedly high rates of delayed surveillance, which could lead to increased risk of dysplastic recurrence and cancer progression. The reasons for delayed surveillance remain unclear. We aimed to identify risk factors for delayed surveillance in patients who successfully completed endoscopic eradication therapy (EET).
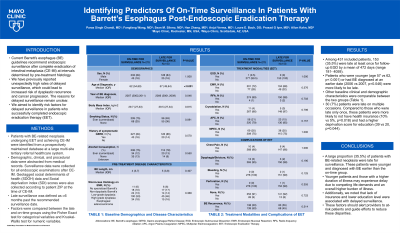
Methods: Patients with BE-related neoplasia undergoing EET and achieving CE-IM were identified from a prospectively maintained database at a large multi-site tertiary referral healthcare system. Demographic, clinical, and procedural data were abstracted from medical records. Surveillance data were collected for all endoscopic examinations after CE-IM. Geotagged social determinants of health (SDOH) data and Social deprivation index (SDI) scores were also collected according to patient ZIP at the time of CE-IM. Late surveillance was defined as >6 months past the recommended surveillance date. Factors were compared between the late and on-time groups using the Fisher Exact test for categorical variables and Kruskal-Wallis test for numeric variables.
Results: Among 431 included patients, 153 (35.5%) were late at least once for follow-up EGD by a mean of 472 days (range 181-4059). Patients who were younger (age 57 vs 62, p< 0.001) or had BE diagnosed at an earlier date (2006 vs 2007, p=0.046) were more likely to be late. Other baseline clinical and demographic characteristics were comparable between the two groups (Table 1). 30 (7%) patients were late on multiple occasions. Compared to those who were late only once, these patients were more likely to not have health insurance (10% vs 5%, p=0.018) and had a higher deprivation score for education (39 vs 20, p=0.044).
Discussion: A large proportion (35.5%) of patients with BE-related neoplasia were late for surveillance. These patients were younger and diagnosed with BE earlier than the on-time group. Younger patients and those with a higher duration of illness may experience delay due to competing life demands and an overall higher burden of illness. Additionally, we noted that lack of insurance and lower education level were associated with delayed surveillance. These factors should alert providers to at-risk patients and guide efforts to reduce these disparities.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Paras Singh Chandi, MBBS1, Fangfang Wang, MD2, Sean Sileno, MD3, Han Zhang, MD4, Anjul Verma, MD1, Laura E. Bach, DO5, Prasad G. Iyer, MD, MS, FACG3, Allon Kahn, MD6. P3903 - Identifying Predictors of On-Time Surveillance in Patients With Barrett’s Esophagus Post-Endoscopic Eradication Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Mayo Clinic Arizona, Scottsdale, AZ; 3Mayo Clinic, Phoenix, AZ; 4Scripps Clinic, La Jolla, CA; 5Mayo Clinic College of Medicine and Science, Oro Valley, AZ; 6Mayo Clinic, Scottsdale, AZ
Introduction: Current Barrett’s esophagus (BE) guidelines recommend endoscopic surveillance after complete eradication of intestinal metaplasia (CE-IM) at intervals determined by pre-treatment histology. We have previously reported unexpectedly high rates of delayed surveillance, which could lead to increased risk of dysplastic recurrence and cancer progression. The reasons for delayed surveillance remain unclear. We aimed to identify risk factors for delayed surveillance in patients who successfully completed endoscopic eradication therapy (EET).
Methods: Patients with BE-related neoplasia undergoing EET and achieving CE-IM were identified from a prospectively maintained database at a large multi-site tertiary referral healthcare system. Demographic, clinical, and procedural data were abstracted from medical records. Surveillance data were collected for all endoscopic examinations after CE-IM. Geotagged social determinants of health (SDOH) data and Social deprivation index (SDI) scores were also collected according to patient ZIP at the time of CE-IM. Late surveillance was defined as >6 months past the recommended surveillance date. Factors were compared between the late and on-time groups using the Fisher Exact test for categorical variables and Kruskal-Wallis test for numeric variables.
Results: Among 431 included patients, 153 (35.5%) were late at least once for follow-up EGD by a mean of 472 days (range 181-4059). Patients who were younger (age 57 vs 62, p< 0.001) or had BE diagnosed at an earlier date (2006 vs 2007, p=0.046) were more likely to be late. Other baseline clinical and demographic characteristics were comparable between the two groups (Table 1). 30 (7%) patients were late on multiple occasions. Compared to those who were late only once, these patients were more likely to not have health insurance (10% vs 5%, p=0.018) and had a higher deprivation score for education (39 vs 20, p=0.044).
Discussion: A large proportion (35.5%) of patients with BE-related neoplasia were late for surveillance. These patients were younger and diagnosed with BE earlier than the on-time group. Younger patients and those with a higher duration of illness may experience delay due to competing life demands and an overall higher burden of illness. Additionally, we noted that lack of insurance and lower education level were associated with delayed surveillance. These factors should alert providers to at-risk patients and guide efforts to reduce these disparities.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Paras Singh Chandi indicated no relevant financial relationships.
Fangfang Wang indicated no relevant financial relationships.
Sean Sileno indicated no relevant financial relationships.
Han Zhang indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Laura Bach indicated no relevant financial relationships.
Prasad G. Iyer: Castle Biosciences – Consultant, Grant/Research Support. CDx Medical – Consultant, Grant/Research Support. Exact Sciences – Advisory Committee/Board Member, Consultant, Grant/Research Support, Intellectual Property/Patents. Medtronic – Consultant. Pentax Medical – Consultant, Grant/Research Support.
Allon Kahn: MiMedx Inc – Consultant.
Paras Singh Chandi, MBBS1, Fangfang Wang, MD2, Sean Sileno, MD3, Han Zhang, MD4, Anjul Verma, MD1, Laura E. Bach, DO5, Prasad G. Iyer, MD, MS, FACG3, Allon Kahn, MD6. P3903 - Identifying Predictors of On-Time Surveillance in Patients With Barrett’s Esophagus Post-Endoscopic Eradication Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
