Tuesday Poster Session
Category: Esophagus
P3907 - The Relationship Between Eosinophilic Esophagitis and Autism Spectrum Disorder in Adult Patients
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SD
Steve D'Souza, MD
Case Western Reserve University / MetroHealth
Cleveland, OH
Presenting Author(s)
Steve D'Souza, MD, Andrew Ford, MD, Noy Lapidot Alon, MD, Ronnie Fass, MD
Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Eosinophilic esophagitis (EoE) is an atopic disorder that is characterized by symptomatic esophageal dysfunction with the presence of an elevated esophageal eosinophil count. Autism spectrum disorder (ASD) is a developmental disorder marked by deficits in social interaction and repetitive patterns of behavior, which are often related to sensory input. Both conditions are associated with feeding dysfunction. Prior work has noted the association between ASD and other gastrointestinal disorders, including GERD. Our aim was to evaluate the relationship between ASD and EoE.
Methods: We used TriNetX, a global collaborative network containing deidentified patient data from the United States and 12 other countries. The incidence of EoE among patients with and without ASD was evaluated. Two cohorts were then examined during a study period of 2000-2023: adult patients with ASD and adult patients with EoE and ASD. Patients with prior foregut surgery, achalasia, connective tissue disorders, and with opiate or GLP-1 agonist use were excluded. We collected data on demographics and generated propensity score matched cohorts for comparison, in order to analyze differences in symptoms, complications, and treatment. Odds ratios and log rank testing were used to evaluate associations between outcomes.
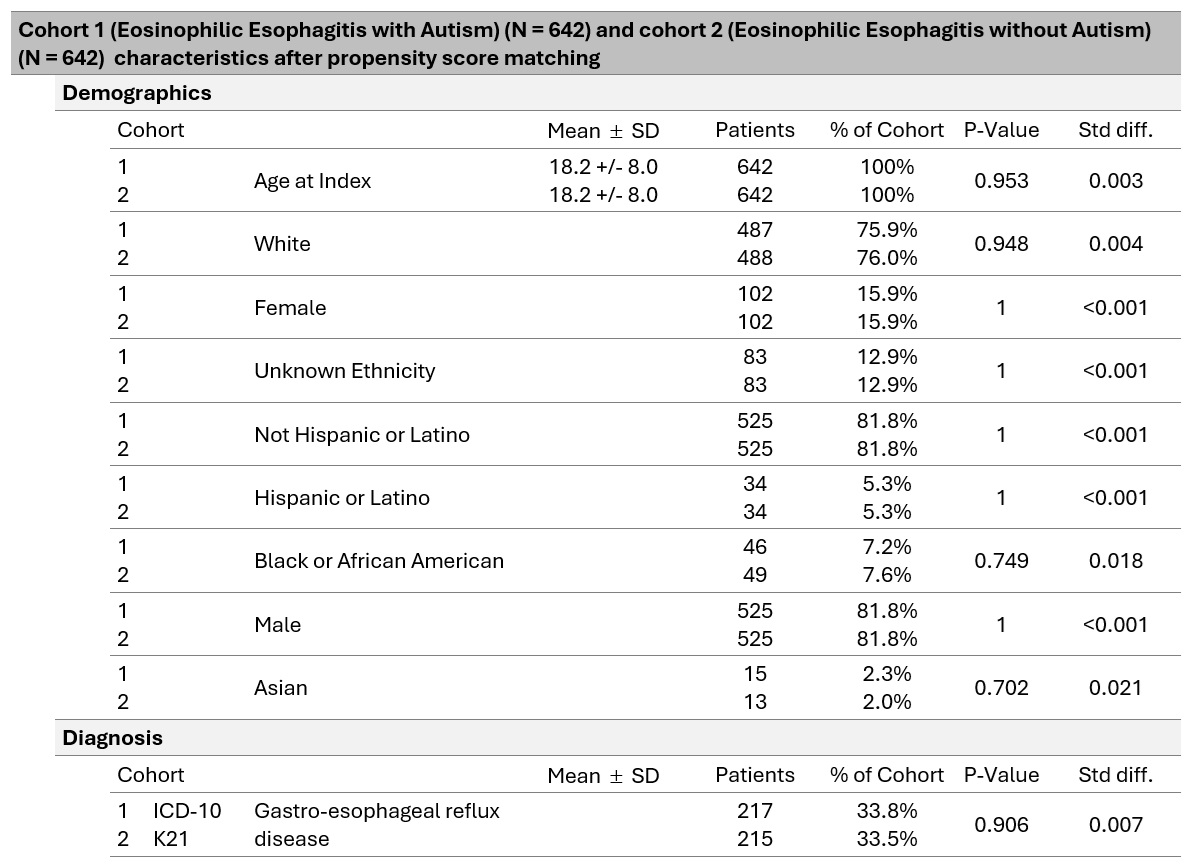
Results: The incidence of EoE was 0.38% in patients with ASD and 0.04% in patients without ASD. After matching, 1284 patients were included in the study, 642 in each cohort. These cohorts were 82% male and 76% white. Patients in the EoE and ASD cohort had higher rates of feeding difficulties (OR=8.61, p< 0.01) but similar rates of dysphagia (OR=0.94, p=0.67) and heartburn (OR=1.20, p=0.67). Moreover, patients with EoE and ASD had higher rates of diagnosis of atopic conditions (OR=1.38, p=0.01) and trended toward more use of PPIs (OR=1.24, p=0.06) and H2RAs (OR=1.38, p=0.09), but had similar rates of dupilumab use (OR 1.07, p=0.86). Complication rates were similar between cohorts, including esophageal stricture (p=0.45), need for dilation (p=0.91), and food impaction (p=0.26).
Discussion: The incidence of EoE is 9.5 times higher in patients with ASD than in those without ASD. Patients with concurrent EoE and ASD have higher rates of food avoidance and medication use than the general EoE population. These differences could be due to several factors, including the potential for delayed or inaccurate diagnosis due to confounding symptoms and higher risk for impaired communication.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Steve D'Souza, MD, Andrew Ford, MD, Noy Lapidot Alon, MD, Ronnie Fass, MD. P3907 - The Relationship Between Eosinophilic Esophagitis and Autism Spectrum Disorder in Adult Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Case Western Reserve University / MetroHealth, Cleveland, OH
Introduction: Eosinophilic esophagitis (EoE) is an atopic disorder that is characterized by symptomatic esophageal dysfunction with the presence of an elevated esophageal eosinophil count. Autism spectrum disorder (ASD) is a developmental disorder marked by deficits in social interaction and repetitive patterns of behavior, which are often related to sensory input. Both conditions are associated with feeding dysfunction. Prior work has noted the association between ASD and other gastrointestinal disorders, including GERD. Our aim was to evaluate the relationship between ASD and EoE.
Methods: We used TriNetX, a global collaborative network containing deidentified patient data from the United States and 12 other countries. The incidence of EoE among patients with and without ASD was evaluated. Two cohorts were then examined during a study period of 2000-2023: adult patients with ASD and adult patients with EoE and ASD. Patients with prior foregut surgery, achalasia, connective tissue disorders, and with opiate or GLP-1 agonist use were excluded. We collected data on demographics and generated propensity score matched cohorts for comparison, in order to analyze differences in symptoms, complications, and treatment. Odds ratios and log rank testing were used to evaluate associations between outcomes.
Results: The incidence of EoE was 0.38% in patients with ASD and 0.04% in patients without ASD. After matching, 1284 patients were included in the study, 642 in each cohort. These cohorts were 82% male and 76% white. Patients in the EoE and ASD cohort had higher rates of feeding difficulties (OR=8.61, p< 0.01) but similar rates of dysphagia (OR=0.94, p=0.67) and heartburn (OR=1.20, p=0.67). Moreover, patients with EoE and ASD had higher rates of diagnosis of atopic conditions (OR=1.38, p=0.01) and trended toward more use of PPIs (OR=1.24, p=0.06) and H2RAs (OR=1.38, p=0.09), but had similar rates of dupilumab use (OR 1.07, p=0.86). Complication rates were similar between cohorts, including esophageal stricture (p=0.45), need for dilation (p=0.91), and food impaction (p=0.26).
Discussion: The incidence of EoE is 9.5 times higher in patients with ASD than in those without ASD. Patients with concurrent EoE and ASD have higher rates of food avoidance and medication use than the general EoE population. These differences could be due to several factors, including the potential for delayed or inaccurate diagnosis due to confounding symptoms and higher risk for impaired communication.
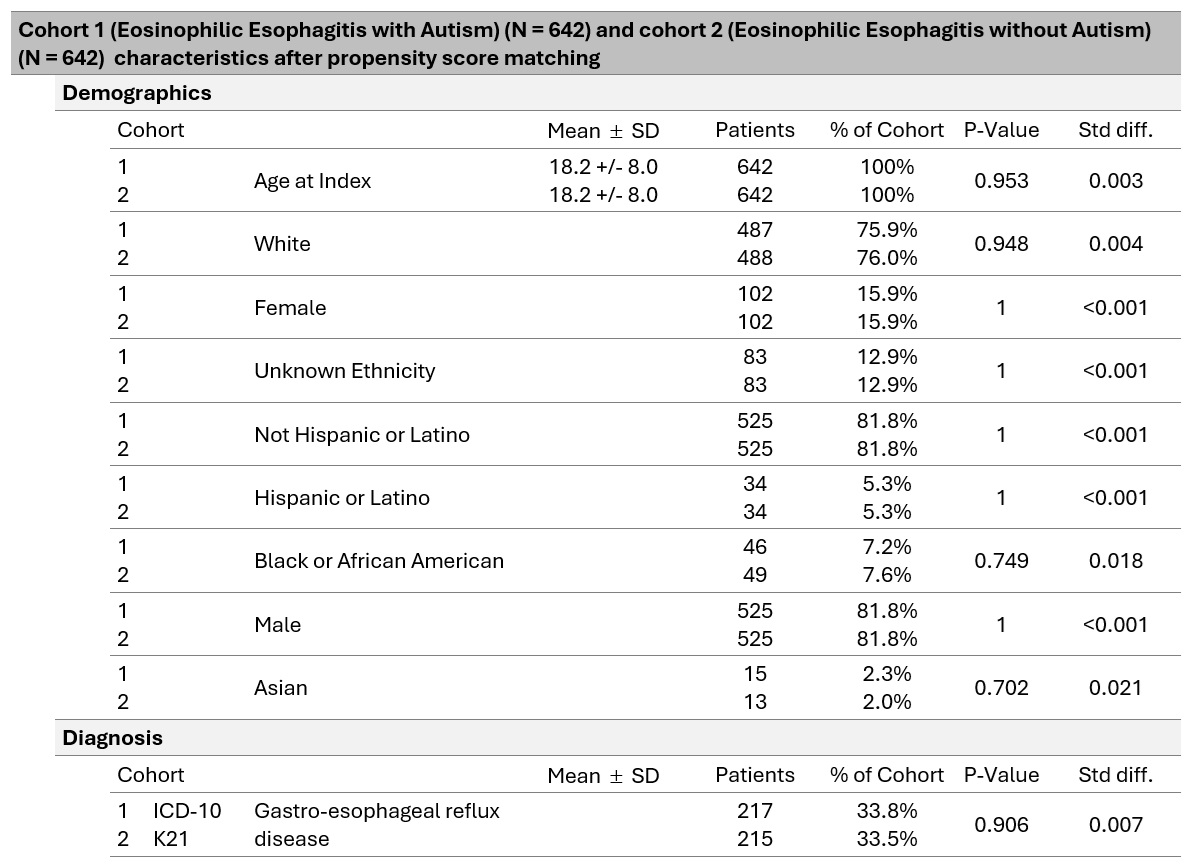
Figure: Figure 1: Characteristics of analyzed cohorts, after propensity score matching.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Steve D'Souza indicated no relevant financial relationships.
Andrew Ford indicated no relevant financial relationships.
Noy Lapidot Alon indicated no relevant financial relationships.
Ronnie Fass indicated no relevant financial relationships.
Steve D'Souza, MD, Andrew Ford, MD, Noy Lapidot Alon, MD, Ronnie Fass, MD. P3907 - The Relationship Between Eosinophilic Esophagitis and Autism Spectrum Disorder in Adult Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
