Tuesday Poster Session
Category: Esophagus
P3919 - Lymphocytic Esophagitis: A Retrospective Multicenter Cohort Study on Natural History, Clinical Profile, and Outcomes
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MP
Maitri Patel, MBBS
GCS Medical College and Research Centre
Ahmedabad, Gujarat, India
Presenting Author(s)
Dhruvkumar Patel, MBBS1, Maitri M. Patel, MBBS2, Lalitkumar Patel, MD3, Dhara Patel, MD2, Shreel H. Patel, MD4, Mukundkumar Patel, MD5
1LSU Health Science Center, Shreveport, LA; 2GCS Medical College and Research Centre, Ahmedabad, Gujarat, India; 3Narendra Modi Medical College, Ahmedabad, Gujarat, India; 4University of Texas Rio Grande Valley - Knapp Medical Center, Weslaco, TX; 5Ananya College of Medicine and Research, Ahmedabad, Gujarat, India
Introduction: Lymphocytic esophagitis, a growing yet poorly understood condition, significantly disrupts daily life. This study aims to elucidate the natural history, clinical presentation, and outcomes of LE in adults.
Methods: We conducted a retrospective review of records for patients aged 18 and older diagnosed with lymphocytic esophagitis at three gastrointestinal clinics between January 2008 and December 2020. We gathered data on demographics, clinical history, lab results, and imaging at diagnosis. A standardized telephone follow-up survey collected additional information on the quality of life, symptom improvement, ER visits, and hospitalizations in the last 5 years.
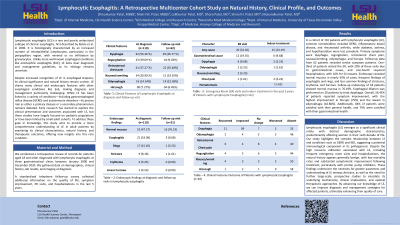
Results: In a cohort of 110 patients with lymphocytic esophagitis (LE), common comorbidities included GERD, inflammatory bowel disease, and rheumatoid arthritis, while diabetes, asthma, and hypothyroidism were less prevalent. Primary symptoms were dysphagia, regurgitation, retrosternal chest pain, nausea/vomiting, odynophagia, and hiccups. Follow-up data from 62 patients revealed similar symptom patterns. One-third of patients visited the ER, with 20% of these visits due to gastrointestinal issues, and one-fourth required hospitalization, with 10% for GI reasons. Endoscopy revealed normal mucosa in nearly 50% of cases, frequent findings of esophagitis and rings, and less common findings of strictures, erythema, and furrows. Follow-up endoscopy of 18 patients showed normal mucosa in 76.19%. Esophageal dilation was performed on 20 patients to treat dysphagia. Overall, 56.45% of patients reported symptom improvement, with the highest improvement in hiccups (75%) and the lowest in odynophagia (42.86%). Additionally, 84% of patients were satisfied with their general health, and 70% were satisfied with their gastrointestinal health.
Discussion: This study highlights that LE is more common in patients with GERD and autoimmune diseases, sharing overlapping clinical and endoscopic features with other esophagitis types. LE generally has a benign course, with most patients achieving symptom relief through lifestyle changes and medical management. Further prospective studies are needed to understand its natural history and explore potential treatments.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Dhruvkumar Patel, MBBS1, Maitri M. Patel, MBBS2, Lalitkumar Patel, MD3, Dhara Patel, MD2, Shreel H. Patel, MD4, Mukundkumar Patel, MD5. P3919 - Lymphocytic Esophagitis: A Retrospective Multicenter Cohort Study on Natural History, Clinical Profile, and Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1LSU Health Science Center, Shreveport, LA; 2GCS Medical College and Research Centre, Ahmedabad, Gujarat, India; 3Narendra Modi Medical College, Ahmedabad, Gujarat, India; 4University of Texas Rio Grande Valley - Knapp Medical Center, Weslaco, TX; 5Ananya College of Medicine and Research, Ahmedabad, Gujarat, India
Introduction: Lymphocytic esophagitis, a growing yet poorly understood condition, significantly disrupts daily life. This study aims to elucidate the natural history, clinical presentation, and outcomes of LE in adults.
Methods: We conducted a retrospective review of records for patients aged 18 and older diagnosed with lymphocytic esophagitis at three gastrointestinal clinics between January 2008 and December 2020. We gathered data on demographics, clinical history, lab results, and imaging at diagnosis. A standardized telephone follow-up survey collected additional information on the quality of life, symptom improvement, ER visits, and hospitalizations in the last 5 years.
Results: In a cohort of 110 patients with lymphocytic esophagitis (LE), common comorbidities included GERD, inflammatory bowel disease, and rheumatoid arthritis, while diabetes, asthma, and hypothyroidism were less prevalent. Primary symptoms were dysphagia, regurgitation, retrosternal chest pain, nausea/vomiting, odynophagia, and hiccups. Follow-up data from 62 patients revealed similar symptom patterns. One-third of patients visited the ER, with 20% of these visits due to gastrointestinal issues, and one-fourth required hospitalization, with 10% for GI reasons. Endoscopy revealed normal mucosa in nearly 50% of cases, frequent findings of esophagitis and rings, and less common findings of strictures, erythema, and furrows. Follow-up endoscopy of 18 patients showed normal mucosa in 76.19%. Esophageal dilation was performed on 20 patients to treat dysphagia. Overall, 56.45% of patients reported symptom improvement, with the highest improvement in hiccups (75%) and the lowest in odynophagia (42.86%). Additionally, 84% of patients were satisfied with their general health, and 70% were satisfied with their gastrointestinal health.
Discussion: This study highlights that LE is more common in patients with GERD and autoimmune diseases, sharing overlapping clinical and endoscopic features with other esophagitis types. LE generally has a benign course, with most patients achieving symptom relief through lifestyle changes and medical management. Further prospective studies are needed to understand its natural history and explore potential treatments.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Dhruvkumar Patel indicated no relevant financial relationships.
Maitri Patel indicated no relevant financial relationships.
Lalitkumar Patel indicated no relevant financial relationships.
Dhara Patel indicated no relevant financial relationships.
Shreel Patel indicated no relevant financial relationships.
Mukundkumar Patel indicated no relevant financial relationships.
Dhruvkumar Patel, MBBS1, Maitri M. Patel, MBBS2, Lalitkumar Patel, MD3, Dhara Patel, MD2, Shreel H. Patel, MD4, Mukundkumar Patel, MD5. P3919 - Lymphocytic Esophagitis: A Retrospective Multicenter Cohort Study on Natural History, Clinical Profile, and Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
