Tuesday Poster Session
Category: Esophagus
P3926 - Robotic-Assisted Versus Video-Assisted Minimally Invasive Surgery for Esophageal Cancer: An Updated Systematic Review, Meta-Analysis and Trial Sequential Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Hasan Al-Obaidi, MD
Jamaica Hospital Medical Center
Briarwood, NY
Presenting Author(s)
Hasan Al-Obaidi, MD1, Eram Shahzadi, MBBS2, Neha Sai Priya Doddapaneni, MBBS3, Shakhnoza Zaynieva, MD4, Mohammed Al-Tawil, MD5
1Jamaica Hospital Medical Center, Briarwood, NY; 2Leighton Hospital MCHFT, Crewe, England, United Kingdom; 3NRI Academy of Medical Sciences, Vijayawada, Andhra Pradesh, India; 4Gabay & Gottlieb Surgery Center, Langhorne, PA; 5Al-Quds University, Jerusalem, Palestinian Territories
Introduction: Esophageal cancer remains a significant global health burden with poor prognosis. Previously open esophagectomy was the preferred surgical modality, but over the past 10 years, minimally invasive esophagectomy has gained popularity. The transition from open esophagectomy to minimally invasive esophagectomy (MIE) is the result of reduced mortality and complications Minimally invasive esophagectomy techniques, including robotic-assisted minimally invasive esophagectomy (RAMIE) and video-assisted minimally invasive esophagectomy (VAMIE), have gained popularity in recent years.
Methods: A comprehensive literature search was conducted on Scopus, EMBASE, and PubMed from inception to September 2023. Randomized controlled trials and propensity-score matched studies comparing RAMIE and VAMIE were included. The updated PRISMA guidelines were followed in conducting this systematic review and meta-analysis.
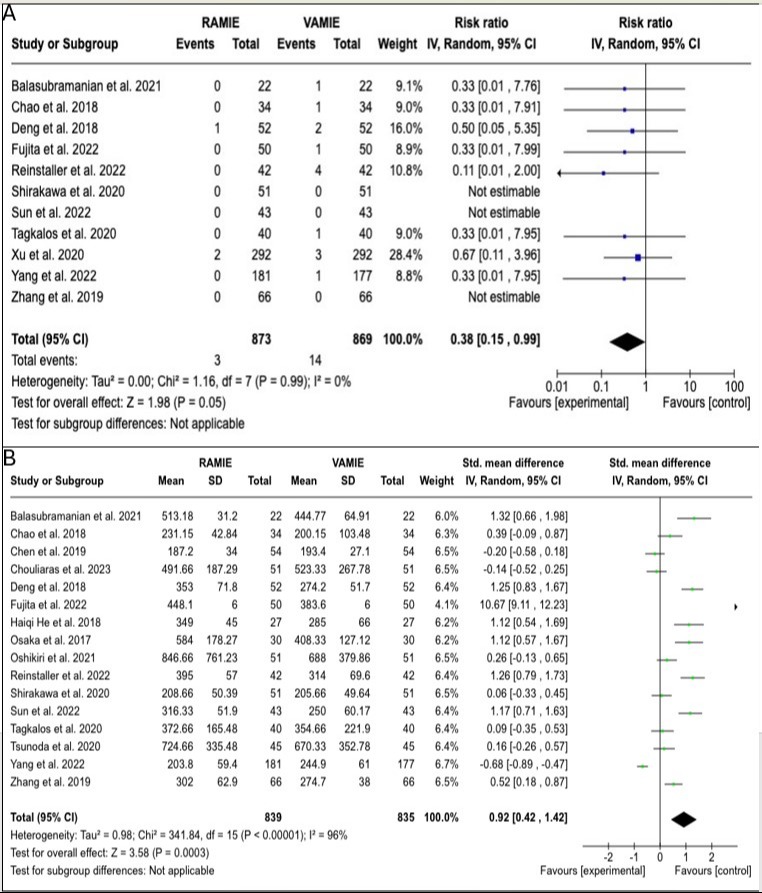
Results: Seventeen studies involving 2258 patients were included. RAMIE was associated with significantly lower short-term all-cause mortality (RR: 0.38, 95% CI: 0.15-0.99, p = 0.05) and reduced pulmonary complications (RR: 0.73, 95% CI: 0.59-0.90, p = 0.003) compared to VAMIE. Additionally, RAMIE showed a lower risk of postoperative chylothorax (RR: 0.52, 95% CI: 0.30-0.89, p = 0.02), decreased total blood loss (SMD: -0.55, 95% CI: -0.95 to -0.15, p = 0.007) and higher number of dissected lymph nodes (SMD:0.12, 95% CI (0.03,0.21), P=0.007). However, RAMIE was associated with longer total operating time (SMD: 0.92, 95% CI: 0.42-1.42, p = 0.0003).
Discussion: Our meta-analysis suggests that RAMIE may offer several clinical advantages over VAME in the treatment of esophageal cancer, including reduced mortality rates, lower incidence of pulmonary complications, and decreased blood loss. However, further studies may be warranted to elucidate the cost-effectiveness and long-term outcomes associated with RAMIE compared to VAME, considering the observed differences in operating time and hospital stay.
Disclosures:
Hasan Al-Obaidi, MD1, Eram Shahzadi, MBBS2, Neha Sai Priya Doddapaneni, MBBS3, Shakhnoza Zaynieva, MD4, Mohammed Al-Tawil, MD5. P3926 - Robotic-Assisted Versus Video-Assisted Minimally Invasive Surgery for Esophageal Cancer: An Updated Systematic Review, Meta-Analysis and Trial Sequential Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Jamaica Hospital Medical Center, Briarwood, NY; 2Leighton Hospital MCHFT, Crewe, England, United Kingdom; 3NRI Academy of Medical Sciences, Vijayawada, Andhra Pradesh, India; 4Gabay & Gottlieb Surgery Center, Langhorne, PA; 5Al-Quds University, Jerusalem, Palestinian Territories
Introduction: Esophageal cancer remains a significant global health burden with poor prognosis. Previously open esophagectomy was the preferred surgical modality, but over the past 10 years, minimally invasive esophagectomy has gained popularity. The transition from open esophagectomy to minimally invasive esophagectomy (MIE) is the result of reduced mortality and complications Minimally invasive esophagectomy techniques, including robotic-assisted minimally invasive esophagectomy (RAMIE) and video-assisted minimally invasive esophagectomy (VAMIE), have gained popularity in recent years.
Methods: A comprehensive literature search was conducted on Scopus, EMBASE, and PubMed from inception to September 2023. Randomized controlled trials and propensity-score matched studies comparing RAMIE and VAMIE were included. The updated PRISMA guidelines were followed in conducting this systematic review and meta-analysis.
Results: Seventeen studies involving 2258 patients were included. RAMIE was associated with significantly lower short-term all-cause mortality (RR: 0.38, 95% CI: 0.15-0.99, p = 0.05) and reduced pulmonary complications (RR: 0.73, 95% CI: 0.59-0.90, p = 0.003) compared to VAMIE. Additionally, RAMIE showed a lower risk of postoperative chylothorax (RR: 0.52, 95% CI: 0.30-0.89, p = 0.02), decreased total blood loss (SMD: -0.55, 95% CI: -0.95 to -0.15, p = 0.007) and higher number of dissected lymph nodes (SMD:0.12, 95% CI (0.03,0.21), P=0.007). However, RAMIE was associated with longer total operating time (SMD: 0.92, 95% CI: 0.42-1.42, p = 0.0003).
Discussion: Our meta-analysis suggests that RAMIE may offer several clinical advantages over VAME in the treatment of esophageal cancer, including reduced mortality rates, lower incidence of pulmonary complications, and decreased blood loss. However, further studies may be warranted to elucidate the cost-effectiveness and long-term outcomes associated with RAMIE compared to VAME, considering the observed differences in operating time and hospital stay.
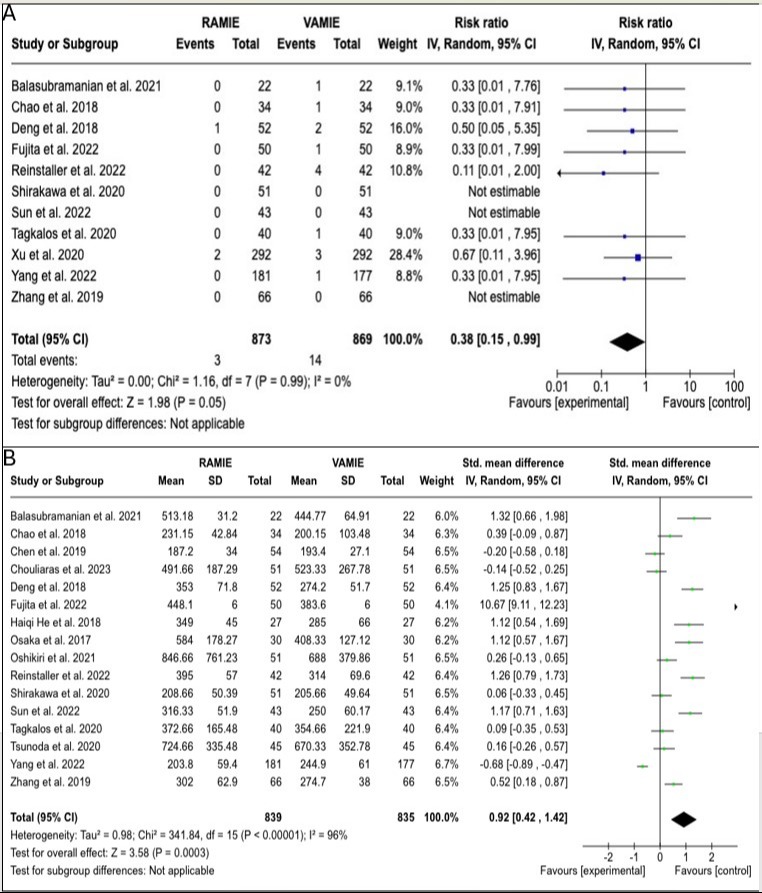
Figure: Figure [A]: Forest plot illustrating short-term mortality (in-hospital or 30-days mortality) following RAMIE versus VAMIE.
Figure [B]: Forest plot illustrating the differences in operative time between patients who underwent RAMIE vs. VAMIE.
Figure [B]: Forest plot illustrating the differences in operative time between patients who underwent RAMIE vs. VAMIE.
Disclosures:
Hasan Al-Obaidi indicated no relevant financial relationships.
Eram Shahzadi indicated no relevant financial relationships.
Neha Sai Priya Doddapaneni indicated no relevant financial relationships.
Shakhnoza Zaynieva indicated no relevant financial relationships.
Mohammed Al-Tawil indicated no relevant financial relationships.
Hasan Al-Obaidi, MD1, Eram Shahzadi, MBBS2, Neha Sai Priya Doddapaneni, MBBS3, Shakhnoza Zaynieva, MD4, Mohammed Al-Tawil, MD5. P3926 - Robotic-Assisted Versus Video-Assisted Minimally Invasive Surgery for Esophageal Cancer: An Updated Systematic Review, Meta-Analysis and Trial Sequential Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
