Tuesday Poster Session
Category: Esophagus
P3940 - The Use of Antidepressants in Patients With Depression Increases the Risk of Gastroesophageal Reflux Disease and Disease Severity
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SS
Sherif Saleh, MD
Case Western Reserve University / MetroHealth
Cleveland, OH
Presenting Author(s)
Sherif Saleh, MD1, Ronnie Fass, MD2
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2MetroHealth Medical Center, Cleveland, OH
Introduction: A few studies have demonstrated an association between Gastroesophageal Reflux Disease (GERD) and depression, with a few reporting that antidepressants may affect lower esophageal sphincter tone and esophageal peristalsis and thus exacerbating reflux. The aim of the study was to evaluate the impact of antidepressants use in patients with depression on GERD and its complications.
Methods: The TriNetX database, which involves 92 healthcare organizations in 12 countries, was utilized for this study. Patients with depression on any antidepressant, on tricyclic antidepressant (TCA) only, on selective serotonin reuptake inhibitors (SSRI) only, or on serotonin and norepinephrine reuptake inhibitors (SNRI) only were evaluated. We performed 1:1 propensity score matching to decrease confounders effects. The prevalence of developing a new diagnosis of GERD and GERD-related complications including erosive esophagitis, esophageal stricture, Barrett's esophagus (BE), BE with dysplasia, and esophageal adenocarcinoma were assessed in each group.
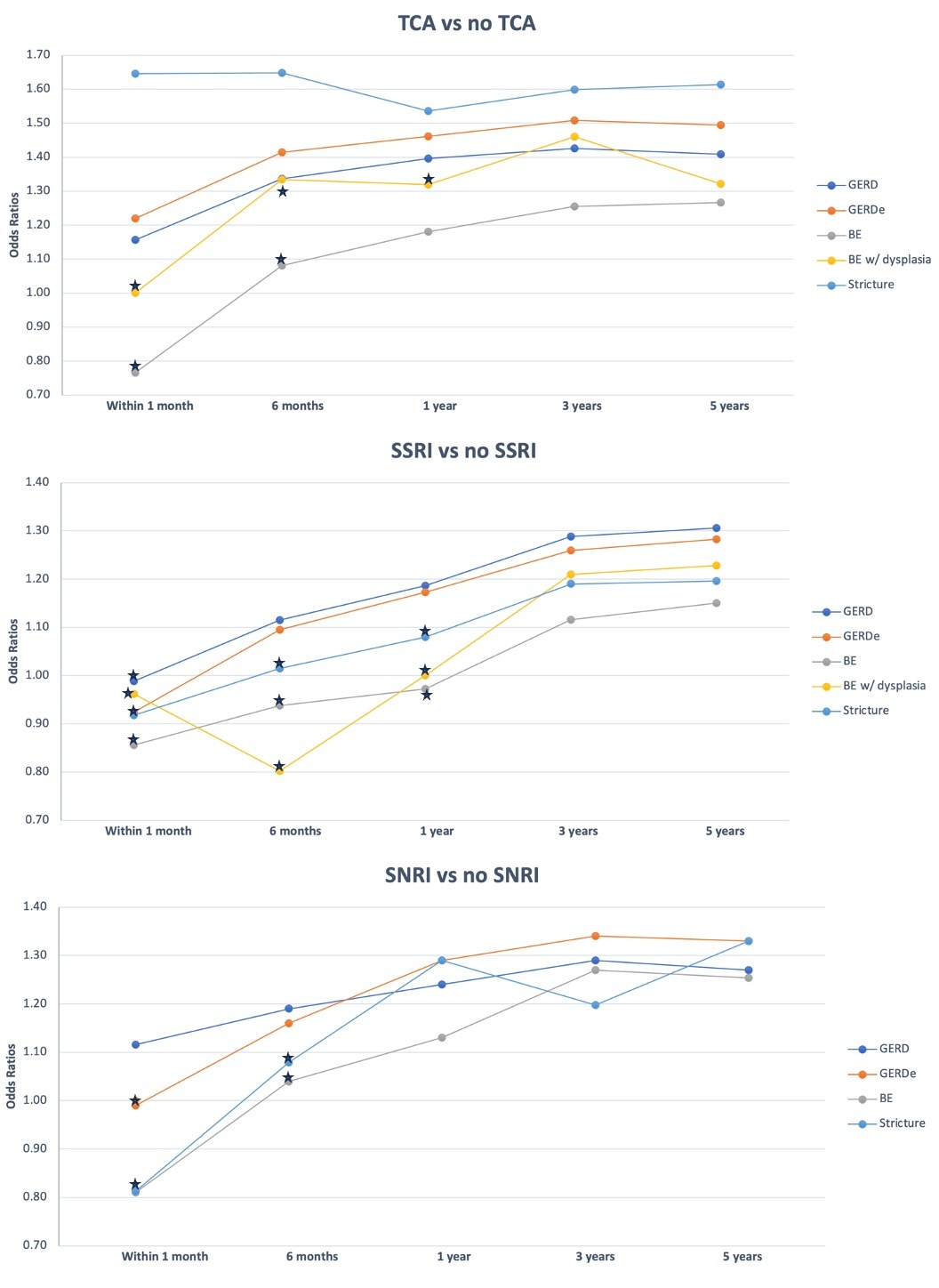
Results: A total of 2,783,790 were included in the antidepressant group, 192,624 in the TCA group, 1,113,795 in the SSRI group, and 432,272 in the SNRI group. The use of TCA compared to those on no TCA was associated with increased risk of developing GERD (OR=1.40, p< 0.01), erosive esophagitis (OR=1.47, p< 0.01), BE (OR=1.24, p< 0.01), BE with dysplasia (OR=1.40, p< 0.01), esophageal stricture (OR=1.53, p< 0.01). The use of SSRI compared to those on no SSRI was associated with increased risk of GERD (OR=1.32, p< 0.01), erosive esophagitis (OR=1.32, p< 0.01), BE (OR=1.14, p< 0.01), BE with dysplasia (OR=1.19, p< 0.01), esophageal stricture (OR=1.21, p< 0.01). The use of SNRI compared to those not no SNRI was associated with increased risk of GERD (OR=1.24, p< 0.01), erosive esophagitis (OR=1.27, p< 0.01), BE (OR=1.20, p< 0.01), BE with dysplasia (OR=1.19, p=0.02), esophageal stricture (OR=1.30, p< 0.01). The risk of GERD and its complications increased with longer use of the aforementioned medications as showed in Figure 1. There was no significantly increased risk in developing esophageal adenocarcinoma with TCA use (OR=1.15, p=0.37), SSRI use (OR=1.04, p=0.59), or SNRI use (OR=1.14, p=0.21).
Discussion: The use of TCA, SSRI and SNRI are all independent risk factors that increase the risk of GERD, erosive esophagitis, BE, BE with dysplasia and esophageal stricture in patients with depression. Among the studied antidepressants, TCA posed the greatest risk.
Disclosures:
Sherif Saleh, MD1, Ronnie Fass, MD2. P3940 - The Use of Antidepressants in Patients With Depression Increases the Risk of Gastroesophageal Reflux Disease and Disease Severity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2MetroHealth Medical Center, Cleveland, OH
Introduction: A few studies have demonstrated an association between Gastroesophageal Reflux Disease (GERD) and depression, with a few reporting that antidepressants may affect lower esophageal sphincter tone and esophageal peristalsis and thus exacerbating reflux. The aim of the study was to evaluate the impact of antidepressants use in patients with depression on GERD and its complications.
Methods: The TriNetX database, which involves 92 healthcare organizations in 12 countries, was utilized for this study. Patients with depression on any antidepressant, on tricyclic antidepressant (TCA) only, on selective serotonin reuptake inhibitors (SSRI) only, or on serotonin and norepinephrine reuptake inhibitors (SNRI) only were evaluated. We performed 1:1 propensity score matching to decrease confounders effects. The prevalence of developing a new diagnosis of GERD and GERD-related complications including erosive esophagitis, esophageal stricture, Barrett's esophagus (BE), BE with dysplasia, and esophageal adenocarcinoma were assessed in each group.
Results: A total of 2,783,790 were included in the antidepressant group, 192,624 in the TCA group, 1,113,795 in the SSRI group, and 432,272 in the SNRI group. The use of TCA compared to those on no TCA was associated with increased risk of developing GERD (OR=1.40, p< 0.01), erosive esophagitis (OR=1.47, p< 0.01), BE (OR=1.24, p< 0.01), BE with dysplasia (OR=1.40, p< 0.01), esophageal stricture (OR=1.53, p< 0.01). The use of SSRI compared to those on no SSRI was associated with increased risk of GERD (OR=1.32, p< 0.01), erosive esophagitis (OR=1.32, p< 0.01), BE (OR=1.14, p< 0.01), BE with dysplasia (OR=1.19, p< 0.01), esophageal stricture (OR=1.21, p< 0.01). The use of SNRI compared to those not no SNRI was associated with increased risk of GERD (OR=1.24, p< 0.01), erosive esophagitis (OR=1.27, p< 0.01), BE (OR=1.20, p< 0.01), BE with dysplasia (OR=1.19, p=0.02), esophageal stricture (OR=1.30, p< 0.01). The risk of GERD and its complications increased with longer use of the aforementioned medications as showed in Figure 1. There was no significantly increased risk in developing esophageal adenocarcinoma with TCA use (OR=1.15, p=0.37), SSRI use (OR=1.04, p=0.59), or SNRI use (OR=1.14, p=0.21).
Discussion: The use of TCA, SSRI and SNRI are all independent risk factors that increase the risk of GERD, erosive esophagitis, BE, BE with dysplasia and esophageal stricture in patients with depression. Among the studied antidepressants, TCA posed the greatest risk.
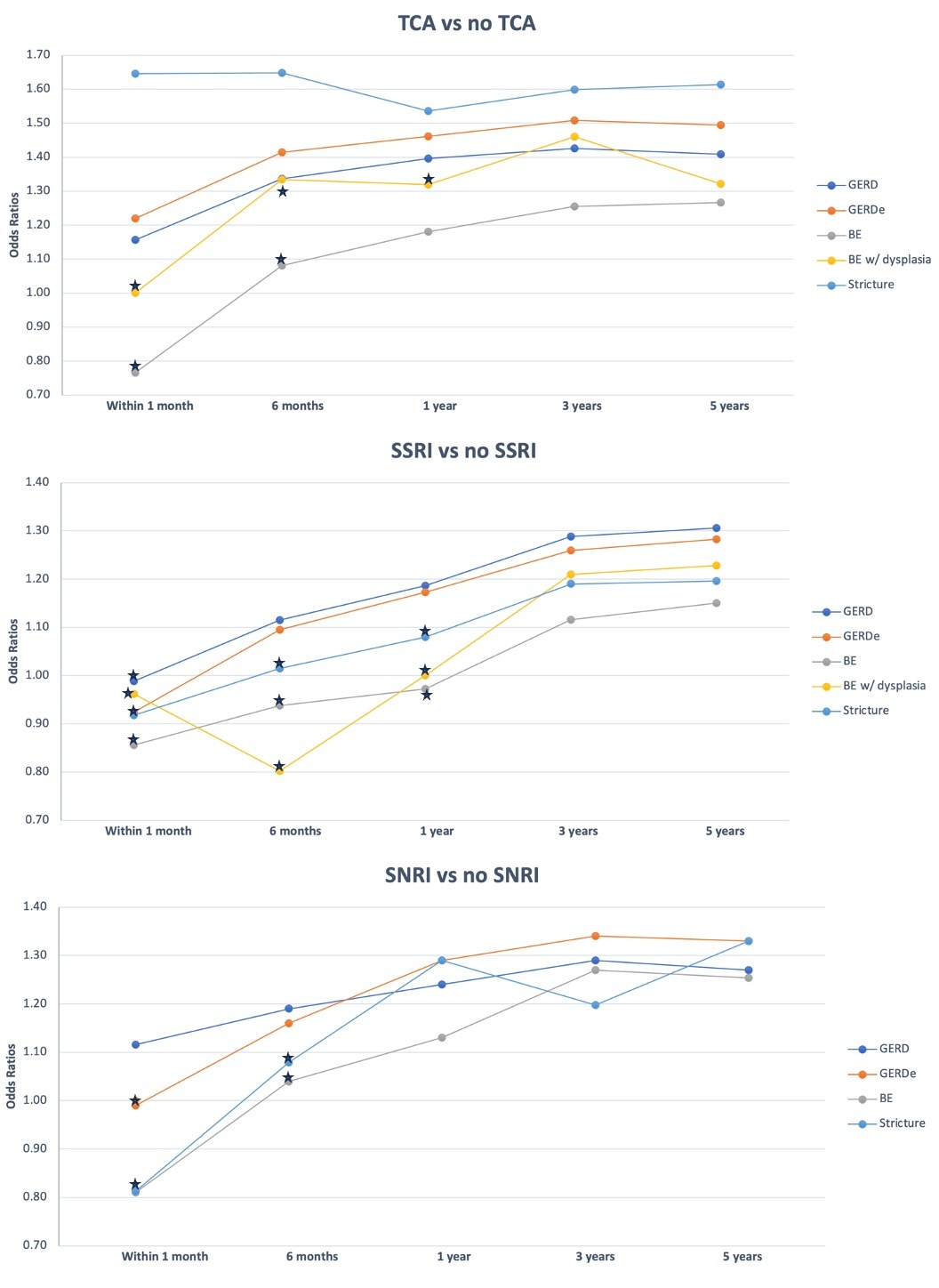
Figure: Table 1: Effect of TCA vs no TCA, SSRI vs no SSRI, SNRI vs no SNRI on GERD and its complications over time in patients with depression
Disclosures:
Sherif Saleh indicated no relevant financial relationships.
Ronnie Fass: Braintree laboratories/Sebela – Advisor or Review Panel Member. carnot – Advisor or Review Panel Member, Speaker. Daewoong – Speaker. Dexcal – Advisor or Review Panel Member. Eisai, Inc. – speaker. GERDCare/Celexio – Advisor or Review Panel Member. Intra-Sana – Speaker. Medicamenta – Speaker. Medtronic – Advisor or Review Panel Member. Phathom Pharmaceuticals – Advisor or Review Panel Member. Restech – Stock Options. Syneos – Advisor or Review Panel Member. Takeda – Speaker.
Sherif Saleh, MD1, Ronnie Fass, MD2. P3940 - The Use of Antidepressants in Patients With Depression Increases the Risk of Gastroesophageal Reflux Disease and Disease Severity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
