Tuesday Poster Session
Category: Esophagus
P3947 - Racial Disparity in Barrett’s Esophagus Screening in Qualifying Females: A Nationwide Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mark Ayoub, MD
West Virginia University - Charleston Area Medical Center
Charleston, WV
Presenting Author(s)
Mark Ayoub, MD1, Carol Faris, MD2, Harleen Chela, MD1, Roberta Hunter, MD1, Ebubekir Daglilar, MD1, Cheryl Cox, MD1
1West Virginia University - Charleston Area Medical Center, Charleston, WV; 2CarePoint Health - Bayonne Medical Center, Charleston, WV
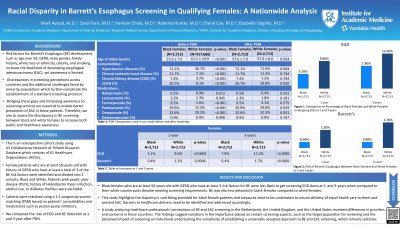
Introduction: Risk factors for Barrett’s Esophagus (BE) development such as age over 50, GERD, male gender, family history, white race or ethnicity, obesity, and smoking increase the likelihood of developing esophageal adenocarcinoma (EAC), yet awareness is limited. Discrepancies in screening perceptions across countries and the additional challenges faced by black and minority populations, such as socioeconomic and systemic healthcare barriers, further complicate the establishment of a standard screening protocol. Bridging these gaps and increasing awareness to screening services are essential to enable better prevention of EAC in those patients. Therefore, we aim to assess the discrepancy in BE screening between black and white females to increase both public and healthcare awareness.
Methods: We queried the US Collaborative Network from TriNetX deidentified research database. Female patients who are at least 50 years old with history of GERD who have at least a total of 3 of the BE risk factors were identified and divided into 2 cohorts; Black and White. Patients with peptic ulcer disease (PUD), history of Helicobacter Pylori infection, alcohol use, or diabetes mellitus were excluded. Cohorts were matched using a 1:1 propensity-scored matching (PSM) based on patients’ comorbidities and medications such as proton pump inhibitors. We compared the rate of EGD and BE detection at 1- and 3-year after PSM.
Results: A total of 420,379 patients met our inclusion criteria. Of those, 0.6% (n=2,713) were black, and 99.4% were white. After PSM, black females had a statistically significant lower rate of screening EGD when compared to their white counterparts at 1 year (5.1% vs 9.6%, p< 0.0001) and 3 years (7.9% vs 12.2%, p< 0.0001). BE detection rate was also lower in black females when compared to white females at 1 year (0.4% vs 1.2%, p=0.0006) and 3 years (0.4% vs 1.7%, p< 0.0001).
Discussion: Black females who are at least 50-years-old with GERD who have at least 3 risk factors for BE were less likely to get screening EGD done at 1- and 3-years when compared to their white counterparts despite meeting screening requirements. BE was also less detected in black females compared to white females. This study highlights the disparity in care being provided for black female patients and measures need to be undertaken to ensure delivery of equal health care to them and prevent EAC. Barriers to healthcare delivery need to be identified and addressed accordingly.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mark Ayoub, MD1, Carol Faris, MD2, Harleen Chela, MD1, Roberta Hunter, MD1, Ebubekir Daglilar, MD1, Cheryl Cox, MD1. P3947 - Racial Disparity in Barrett’s Esophagus Screening in Qualifying Females: A Nationwide Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1West Virginia University - Charleston Area Medical Center, Charleston, WV; 2CarePoint Health - Bayonne Medical Center, Charleston, WV
Introduction: Risk factors for Barrett’s Esophagus (BE) development such as age over 50, GERD, male gender, family history, white race or ethnicity, obesity, and smoking increase the likelihood of developing esophageal adenocarcinoma (EAC), yet awareness is limited. Discrepancies in screening perceptions across countries and the additional challenges faced by black and minority populations, such as socioeconomic and systemic healthcare barriers, further complicate the establishment of a standard screening protocol. Bridging these gaps and increasing awareness to screening services are essential to enable better prevention of EAC in those patients. Therefore, we aim to assess the discrepancy in BE screening between black and white females to increase both public and healthcare awareness.
Methods: We queried the US Collaborative Network from TriNetX deidentified research database. Female patients who are at least 50 years old with history of GERD who have at least a total of 3 of the BE risk factors were identified and divided into 2 cohorts; Black and White. Patients with peptic ulcer disease (PUD), history of Helicobacter Pylori infection, alcohol use, or diabetes mellitus were excluded. Cohorts were matched using a 1:1 propensity-scored matching (PSM) based on patients’ comorbidities and medications such as proton pump inhibitors. We compared the rate of EGD and BE detection at 1- and 3-year after PSM.
Results: A total of 420,379 patients met our inclusion criteria. Of those, 0.6% (n=2,713) were black, and 99.4% were white. After PSM, black females had a statistically significant lower rate of screening EGD when compared to their white counterparts at 1 year (5.1% vs 9.6%, p< 0.0001) and 3 years (7.9% vs 12.2%, p< 0.0001). BE detection rate was also lower in black females when compared to white females at 1 year (0.4% vs 1.2%, p=0.0006) and 3 years (0.4% vs 1.7%, p< 0.0001).
Discussion: Black females who are at least 50-years-old with GERD who have at least 3 risk factors for BE were less likely to get screening EGD done at 1- and 3-years when compared to their white counterparts despite meeting screening requirements. BE was also less detected in black females compared to white females. This study highlights the disparity in care being provided for black female patients and measures need to be undertaken to ensure delivery of equal health care to them and prevent EAC. Barriers to healthcare delivery need to be identified and addressed accordingly.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mark Ayoub indicated no relevant financial relationships.
Carol Faris indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Roberta Hunter indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Cheryl Cox indicated no relevant financial relationships.
Mark Ayoub, MD1, Carol Faris, MD2, Harleen Chela, MD1, Roberta Hunter, MD1, Ebubekir Daglilar, MD1, Cheryl Cox, MD1. P3947 - Racial Disparity in Barrett’s Esophagus Screening in Qualifying Females: A Nationwide Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
