Tuesday Poster Session
Category: Esophagus
P3955 - A Rare Case of Pancreatic Cancer Causing Secondary Achalasia
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
- HO
Haya Omeish, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Haya Omeish, MD1, Ammad Javaid. Chaudhary, MD1, Taher Jamali, MD2, Abdulmalik Saleem, MD1, Muhammad Zarrar Khan, MD3
1Henry Ford Health, Detroit, MI; 2Henry Ford Hospital, Detroit, MI; 3Henry Ford Hospital, Royal Oak, MI
Introduction: Secondary achalasia or Pseudoachalasia is a rare esophageal motility disorder resembling idiopathic achalasia. Most pseudoachalasia cases involve neoplasia at or near the esophagogastric (EG) junction. Pancreatic cancer rarely causes pseudoachalasia. This disorder may result from circumferential obstruction of the distal esophagus or malignant infiltration destroying inhibitory neurons. We present a rare case of pseudoachalasia caused by pancreatic cancer highlights the need to consider malignancies beyond the EG junction in diagnosis.
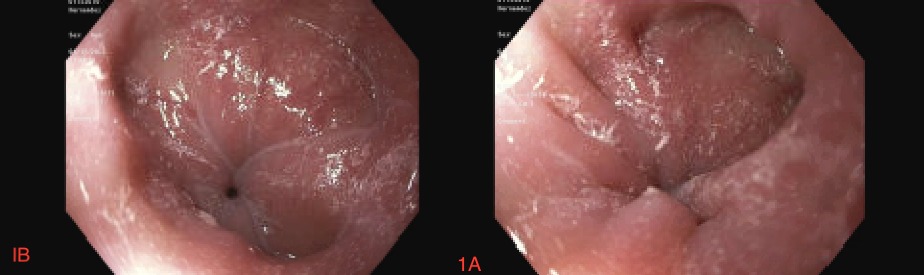
Case Description/Methods: A 77-year-old female with a history of pancreatic adenocarcinoma presented with a six-month history of dysphagia, abdominal pain, and a 30 lb weight loss over three months. Laboratory findings revealed leukocytosis, high anion gap metabolic acidosis due to starvation ketosis, and elevated liver enzymes (AST 299 U/L, ALT 384 U/L, alkaline phosphatase 942 IU/L). A CT scan of the abdomen showed progression of the pancreatic head mass, encasing vascular structures, worsening biliary duct dilation, centrally necrotic mesenteric lymph nodes, and new small ascites. An esophagogram revealed significant narrowing of the distal esophagus, gastroesophageal junction, and proximal stomach. An EGD with ERCP demonstrated type 3 achalasia and a single moderate localized malignant biliary stricture treated with biliary sphincterotomy and stent placement.
The patient received five cycles of radiation therapy followed by resumption of chemotherapy. Due to declining health and comorbidities, further pancreatic cancer treatment was considered inappropriate. After discussion with the patient and family, they opted for hospice care, and the patient passed away five months later.
Discussion: This case underscores the critical need to broaden the differential diagnosis when evaluating patients with unexplained dysphagia. While rare, pseudoachalasia, which has been associated with pancreatic cancer in only four reported cases, should be considered in such patients. When standard treatments fail to alleviate symptoms in typical achalasia cases, secondary achalasia may be suspected.
Disclosures:
Haya Omeish, MD1, Ammad Javaid. Chaudhary, MD1, Taher Jamali, MD2, Abdulmalik Saleem, MD1, Muhammad Zarrar Khan, MD3. P3955 - A Rare Case of Pancreatic Cancer Causing Secondary Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2Henry Ford Hospital, Detroit, MI; 3Henry Ford Hospital, Royal Oak, MI
Introduction: Secondary achalasia or Pseudoachalasia is a rare esophageal motility disorder resembling idiopathic achalasia. Most pseudoachalasia cases involve neoplasia at or near the esophagogastric (EG) junction. Pancreatic cancer rarely causes pseudoachalasia. This disorder may result from circumferential obstruction of the distal esophagus or malignant infiltration destroying inhibitory neurons. We present a rare case of pseudoachalasia caused by pancreatic cancer highlights the need to consider malignancies beyond the EG junction in diagnosis.
Case Description/Methods: A 77-year-old female with a history of pancreatic adenocarcinoma presented with a six-month history of dysphagia, abdominal pain, and a 30 lb weight loss over three months. Laboratory findings revealed leukocytosis, high anion gap metabolic acidosis due to starvation ketosis, and elevated liver enzymes (AST 299 U/L, ALT 384 U/L, alkaline phosphatase 942 IU/L). A CT scan of the abdomen showed progression of the pancreatic head mass, encasing vascular structures, worsening biliary duct dilation, centrally necrotic mesenteric lymph nodes, and new small ascites. An esophagogram revealed significant narrowing of the distal esophagus, gastroesophageal junction, and proximal stomach. An EGD with ERCP demonstrated type 3 achalasia and a single moderate localized malignant biliary stricture treated with biliary sphincterotomy and stent placement.
The patient received five cycles of radiation therapy followed by resumption of chemotherapy. Due to declining health and comorbidities, further pancreatic cancer treatment was considered inappropriate. After discussion with the patient and family, they opted for hospice care, and the patient passed away five months later.
Discussion: This case underscores the critical need to broaden the differential diagnosis when evaluating patients with unexplained dysphagia. While rare, pseudoachalasia, which has been associated with pancreatic cancer in only four reported cases, should be considered in such patients. When standard treatments fail to alleviate symptoms in typical achalasia cases, secondary achalasia may be suspected.
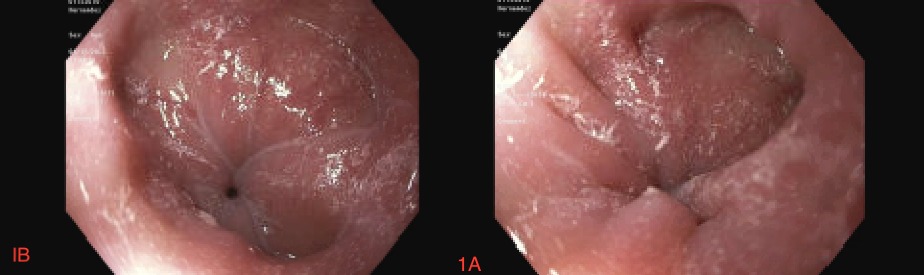
Figure: Figure-1A and 1B: EGD suggestive of type 3 achalasia
Disclosures:
Haya Omeish indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Taher Jamali indicated no relevant financial relationships.
Abdulmalik Saleem indicated no relevant financial relationships.
Muhammad Zarrar Khan indicated no relevant financial relationships.
Haya Omeish, MD1, Ammad Javaid. Chaudhary, MD1, Taher Jamali, MD2, Abdulmalik Saleem, MD1, Muhammad Zarrar Khan, MD3. P3955 - A Rare Case of Pancreatic Cancer Causing Secondary Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
