Tuesday Poster Session
Category: Esophagus
P3956 - A Case of Co-Existing Eosinophilic Esophagitis and Type II Achalasia
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Brandon Truong, MD
Cedars-Sinai Medical Center
Los Angeles, CA
Presenting Author(s)
Brandon Truong, MD, Benjamin Basseri, MD, Richard Sukov, MD, FACR, Rabindra Watson, MD, Amrit K.. Kamboj, MD
Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Dysphagia is a common presenting complaint to the gastroenterology clinic and can occur due to structural causes, such as eosinophilic esophagitis (EoE) and motility disorders, including achalasia. While a single etiology typically accounts for the dysphagia, rarely, two separate disorders can contribute as highlighted in this patient case.
Case Description/Methods: A 55-year-old woman presented with eight months of dysphagia to solids. She underwent an esophagogastroduodenoscopy (EGD) with normal appearing esophagus with esophageal biopsies demonstrating 70-80 eosinophils per high powered field (eos/HPF) consistent with EoE. She was initially treated with elimination diets, omeprazole, and oral topical corticosteroids, but continued to have progressively worsening dysphagia to both solids and liquids with a 14-pound weight loss, along with persistent eosinophilia on esophageal biopsies. She was then initiated on weekly dupilumab and achieved histologic remission; however, she continued to have worsening dysphagia. Six months after starting dupilumab, she underwent high-resolution esophageal manometry (HRM) which revealed esophagogastric junction outlet obstruction. Repeat EGD demonstrated 5 eos/HPF in the esophagus without stricture and Botox injection was administered to the distal esophagus and lower esophageal sphincter with significant improvement in symptoms for four months. Unfortunately, her symptoms progressed thereafter requiring multiple emergency department visits for intravenous hydration. One year after Botox injection, a timed barium esophagram was performed which demonstrated bird's beak appearance at the lower esophageal sphincter suspicious for achalasia. Repeat HRM was consistent with Type II achalasia. Ultimately, the patient underwent an uncomplicated peroral endoscopic myotomy (POEM). Superficial muscle biopsies performed at time of POEM did not show any eosinophils. At follow-up one week later, she reported near complete resolution of dysphagia.
Discussion: Here, we highlight a patient case with a biopsy-proven diagnosis of EoE that achieved histologic remission with dupilumab but continued to have worsening dysphagia symptoms. Additional work-up led to a diagnosis of type II achalasia that was adequately treated with POEM with good symptom response. While EoE and achalasia are well-established etiologies of dysphagia, this case reinforces findings from recent studies that suggest achalasia may be strongly associated with EoE

Disclosures:
Brandon Truong, MD, Benjamin Basseri, MD, Richard Sukov, MD, FACR, Rabindra Watson, MD, Amrit K.. Kamboj, MD. P3956 - A Case of Co-Existing Eosinophilic Esophagitis and Type II Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Cedars-Sinai Medical Center, Los Angeles, CA
Introduction: Dysphagia is a common presenting complaint to the gastroenterology clinic and can occur due to structural causes, such as eosinophilic esophagitis (EoE) and motility disorders, including achalasia. While a single etiology typically accounts for the dysphagia, rarely, two separate disorders can contribute as highlighted in this patient case.
Case Description/Methods: A 55-year-old woman presented with eight months of dysphagia to solids. She underwent an esophagogastroduodenoscopy (EGD) with normal appearing esophagus with esophageal biopsies demonstrating 70-80 eosinophils per high powered field (eos/HPF) consistent with EoE. She was initially treated with elimination diets, omeprazole, and oral topical corticosteroids, but continued to have progressively worsening dysphagia to both solids and liquids with a 14-pound weight loss, along with persistent eosinophilia on esophageal biopsies. She was then initiated on weekly dupilumab and achieved histologic remission; however, she continued to have worsening dysphagia. Six months after starting dupilumab, she underwent high-resolution esophageal manometry (HRM) which revealed esophagogastric junction outlet obstruction. Repeat EGD demonstrated 5 eos/HPF in the esophagus without stricture and Botox injection was administered to the distal esophagus and lower esophageal sphincter with significant improvement in symptoms for four months. Unfortunately, her symptoms progressed thereafter requiring multiple emergency department visits for intravenous hydration. One year after Botox injection, a timed barium esophagram was performed which demonstrated bird's beak appearance at the lower esophageal sphincter suspicious for achalasia. Repeat HRM was consistent with Type II achalasia. Ultimately, the patient underwent an uncomplicated peroral endoscopic myotomy (POEM). Superficial muscle biopsies performed at time of POEM did not show any eosinophils. At follow-up one week later, she reported near complete resolution of dysphagia.
Discussion: Here, we highlight a patient case with a biopsy-proven diagnosis of EoE that achieved histologic remission with dupilumab but continued to have worsening dysphagia symptoms. Additional work-up led to a diagnosis of type II achalasia that was adequately treated with POEM with good symptom response. While EoE and achalasia are well-established etiologies of dysphagia, this case reinforces findings from recent studies that suggest achalasia may be strongly associated with EoE

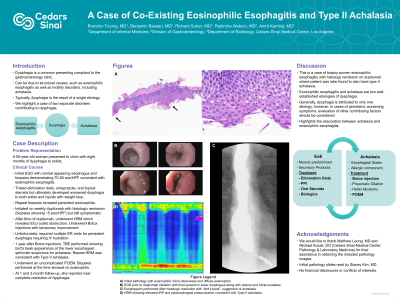
Figure: Figure: A) EGD prior to initiation of dupilumab showing food in the lower third of the esophagus with diffuse, white plaques with biopsies showing up to 57 eos/hpf, including eosinophilic micro-abscesses, consistent with eosinophilic esophagitis. No candida was noted on pathology. B) Esophagram performed 18 months after initiation of dupilumab demonstrating a “bird’s beak” appearance at the level of the lower esophageal sphincter, suggestive of achalasia. C) HRM performed one month after esophagram showing elevated IRP and panesophageal pressurization consistent with Type II achalasia.
Disclosures:
Brandon Truong indicated no relevant financial relationships.
Benjamin Basseri indicated no relevant financial relationships.
Richard Sukov indicated no relevant financial relationships.
Rabindra Watson: Allurion – Grant/Research Support. Ambu Inc – Consultant. Apollo Endosurgery – Consultant, Speakers Bureau. Boston scientific – Consultant, Speakers Bureau. Intuitive surgical – Advisory Committee/Board Member.
Amrit Kamboj: Castle Biosciences – Consultant.
Brandon Truong, MD, Benjamin Basseri, MD, Richard Sukov, MD, FACR, Rabindra Watson, MD, Amrit K.. Kamboj, MD. P3956 - A Case of Co-Existing Eosinophilic Esophagitis and Type II Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
