Tuesday Poster Session
Category: Esophagus
P3964 - Herpes Esophagitis Presenting as an Upper Gastrointestinal Bleed in an Immunocompetent Geriatric Male
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RP
Rahul Patel, DO
Jefferson Health
Washington Township, NJ
Presenting Author(s)
Rahul Patel, DO, Edward Bley, DO, Joshua Soliman, DO, Luna Li, MD, PhD, Richard Walters, DO
Jefferson Health, Washington Township, NJ
Introduction: Infectious esophagitis is typically seen in patients with immunosuppression. We present a case of newly diagnosed herpes esophagitis presenting as an upper gastrointestinal bleed (UGI) in an immunocompetent male.
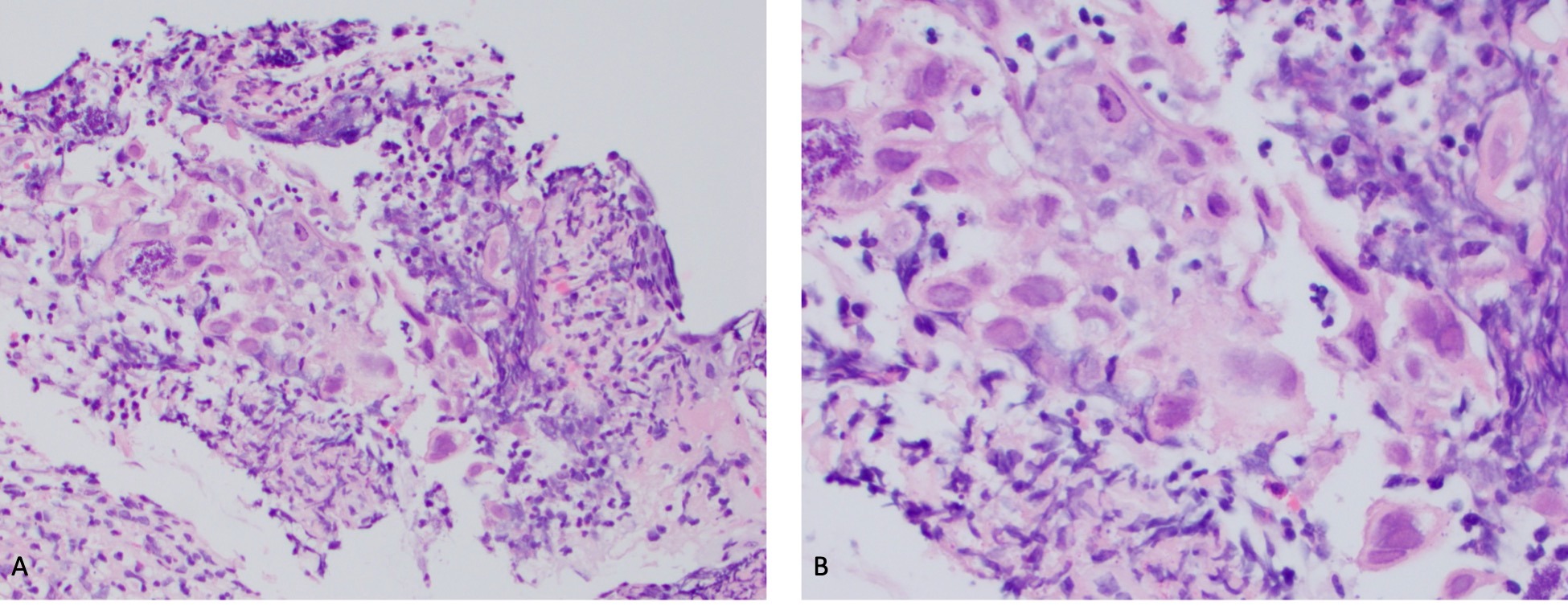
Case Description/Methods: 82-year-old male with a history of Alzheimer’s dementia, normal pressure hydrocephalus status post ventriculoperitoneal shunt (VPS), atrial fibrillation, recent right middle cerebral artery embolic stroke was brought to the hospital from rehab for altered mentation. A repeat MRI was done showing large acute right anterior circulation infarcts. When he arrived to this hospital, neurology started him clopidogrel 75mg daily in addition to the aspirin he was on with a direct acting oral anticoagulant deferred until post stroke day 10. Gastroenterology became involved in his care 7 days into his hospitalization for normocytic anemia. His hemoglobin on arrival was 14.6 g/dL. By the time gastroenterology was consulted, it was 7.0 g/dL. Iron studies, B12 and folate were unremarkable. Haptoglobin, lactate dehydrogenase, and reticulocyte labs were not consistent with a hemolytic process. He did not have hemodynamic instability, gastrointestinal symptoms or overt bleeding. His oral mucosa was unremarkable. He denied odynophagia and dysphagia but nursing had concerns about swallowing function. Initially, his family deferred an endoscopic evaluation so he was managed with pantoprazole 40mg twice a day. After 2 days and 3 units of packed red blood cell transfusions, the family wished to proceed with an esophagogastroduodenoscopy (EGD). EGD showed grade D esophagitis along the entire esophagus. Stomach and duodenum were unremarkable. He was then started on sucralfate. Esophageal biopsy results showed acute inflammation and granulation tissue with focal cytopathic viral effect consistent with herpes esophagitis (figure 1). He tested negative for human immunodeficiency virus. He was managed with acyclovir with hemoglobin stability noted.
Discussion: This case demonstrated an atypical presentation of an UGI bleed. HSV esophagitis is seldom seen in immunocompetent individuals. Furthermore, the most common clinical features are odynophagia, oral mucosal lesions, regurgitation, and systemic signs of infection. Our case is of interest because our patient did not exhibit any of those symptoms and he was immunocompetent. Observing his rapid hemoglobin improvement after starting anti-viral therapy with acyclovir was remarkable.
Disclosures:
Rahul Patel, DO, Edward Bley, DO, Joshua Soliman, DO, Luna Li, MD, PhD, Richard Walters, DO. P3964 - Herpes Esophagitis Presenting as an Upper Gastrointestinal Bleed in an Immunocompetent Geriatric Male, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Jefferson Health, Washington Township, NJ
Introduction: Infectious esophagitis is typically seen in patients with immunosuppression. We present a case of newly diagnosed herpes esophagitis presenting as an upper gastrointestinal bleed (UGI) in an immunocompetent male.
Case Description/Methods: 82-year-old male with a history of Alzheimer’s dementia, normal pressure hydrocephalus status post ventriculoperitoneal shunt (VPS), atrial fibrillation, recent right middle cerebral artery embolic stroke was brought to the hospital from rehab for altered mentation. A repeat MRI was done showing large acute right anterior circulation infarcts. When he arrived to this hospital, neurology started him clopidogrel 75mg daily in addition to the aspirin he was on with a direct acting oral anticoagulant deferred until post stroke day 10. Gastroenterology became involved in his care 7 days into his hospitalization for normocytic anemia. His hemoglobin on arrival was 14.6 g/dL. By the time gastroenterology was consulted, it was 7.0 g/dL. Iron studies, B12 and folate were unremarkable. Haptoglobin, lactate dehydrogenase, and reticulocyte labs were not consistent with a hemolytic process. He did not have hemodynamic instability, gastrointestinal symptoms or overt bleeding. His oral mucosa was unremarkable. He denied odynophagia and dysphagia but nursing had concerns about swallowing function. Initially, his family deferred an endoscopic evaluation so he was managed with pantoprazole 40mg twice a day. After 2 days and 3 units of packed red blood cell transfusions, the family wished to proceed with an esophagogastroduodenoscopy (EGD). EGD showed grade D esophagitis along the entire esophagus. Stomach and duodenum were unremarkable. He was then started on sucralfate. Esophageal biopsy results showed acute inflammation and granulation tissue with focal cytopathic viral effect consistent with herpes esophagitis (figure 1). He tested negative for human immunodeficiency virus. He was managed with acyclovir with hemoglobin stability noted.
Discussion: This case demonstrated an atypical presentation of an UGI bleed. HSV esophagitis is seldom seen in immunocompetent individuals. Furthermore, the most common clinical features are odynophagia, oral mucosal lesions, regurgitation, and systemic signs of infection. Our case is of interest because our patient did not exhibit any of those symptoms and he was immunocompetent. Observing his rapid hemoglobin improvement after starting anti-viral therapy with acyclovir was remarkable.
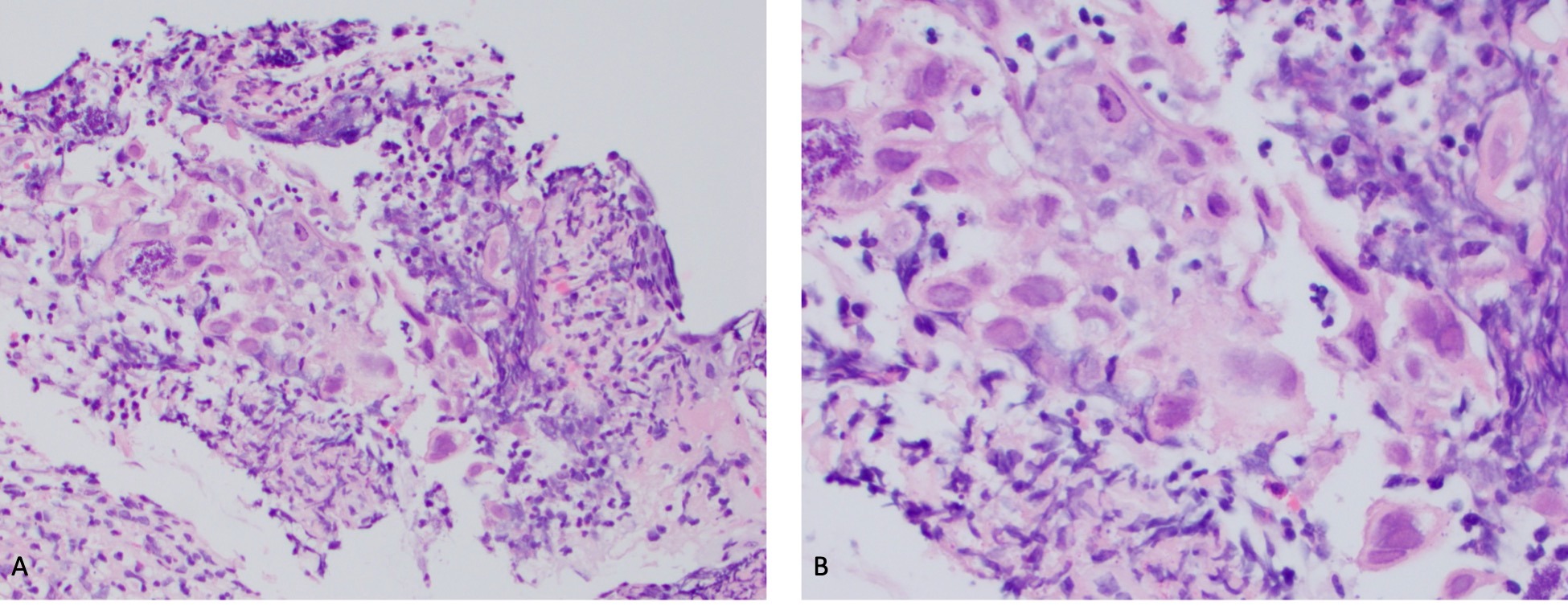
Figure: Figure 1: Specimen shows squamous mucosa with inflammation/granulation tissue with focal cytopathic viral effect, including enlarged and multinucleated cells, nuclear molding and chromatin margination. HSV1-II immunochemical stain positivity. CMV is negative. Negative intestinal metaplasia or fungal elements.
A-200x
B-400x
A-200x
B-400x
Disclosures:
Rahul Patel indicated no relevant financial relationships.
Edward Bley indicated no relevant financial relationships.
Joshua Soliman indicated no relevant financial relationships.
Luna Li indicated no relevant financial relationships.
Richard Walters indicated no relevant financial relationships.
Rahul Patel, DO, Edward Bley, DO, Joshua Soliman, DO, Luna Li, MD, PhD, Richard Walters, DO. P3964 - Herpes Esophagitis Presenting as an Upper Gastrointestinal Bleed in an Immunocompetent Geriatric Male, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
