Tuesday Poster Session
Category: Endoscopy Video Forum
P3889 - Modified Endoscopic Submucosal Dissection (ESD) With Suturing for the Treatment of Gastro-Gastric Fistula
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Noppachai Siranart, MD
Brigham and Women's Hospital
Boston, MA
Presenting Author(s)
Noppachai Siranart, MD1, Christopher C.. Thompson, MD, MSc2, Pichamol Jirapinyo, MD, MPH3
1Brigham and Women's Hospital, Boston, MA; 2Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 3Brigham and Women's Hospital, Boston, MA
Introduction: Gastro-gastric fistulae (GGF) may occur in upto 6% of patients following Roux-en-Y gastric bypass (RYGB). Various endoscopic approaches to treat GGF have been described including endoscopic suturing. Nevertheless, the efficacy of suturing at treating GGF, especially for those with a diameter of >1 cm, remains suboptimal. Here, we present a case of a large GGF treated with a combined endoscopic submucosal dissection (ESD) with suturing technique, aimed at improving efficacy and durability results.
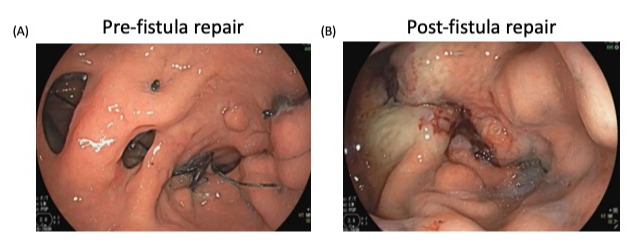
Case Description/Methods: A 53-year-old woman with a history of open Roux-en-Y gastric bypass in 2003 status post endoscopic revision of RYGB via a plication technique (i.e. ROSE procedure) in 2021, complicated by gastrojejunal anastomosis (GJA) stenosis treated successfully with a balloon dilation, who presented with reflux and weight regain. An upper gastrointestinal study revealed a GGF. On an endoscopy, 2 GGF were seen on the left side of the pouch measuring 12 mm and 16 mm in diameter. Given the large sizes of both GGFs, the decision was made to close them with a combined ESD with suturing technique. First, ESD was performed around the GGF to prepare the tissue prior to endoscopic suturing. Specifically, mucosal incision was performed circumferentially around the GJA using an injection knife. The dissected area was then trimmed to widen and expose the submucosal and/or muscular layer using the same injection knife. Argon plasma coagulation was then performed on the inner and outer rims of the dissected area. Suturing was then performed using a running suture pattern by placing stitches from the inside of the GGF through the exposed submucosal/muscular layer to close the GGF. Once the first GGF was closed, the same steps were repeated to close the second, distal GGF (Video). At the end of the procedure, both GGFs were closed successfully. There were no intra or post-procedural adverse events. At the 2-month follow-up, her weight decreased from 208 to 194 lbs, representing a 6.7% TWL. She reported resolution of reflux symptoms and was able to discontinue a proton pump inhibitor. A follow-up upper gastrointestinal study confirmed successful closure of both GGFs.
Discussion: Combining ESD with suturing is technically feasible and effective technique at treating GGF in patients with RYGB. Further studies are warranted to assess the durability of this novel technique.
Disclosures:
Noppachai Siranart, MD1, Christopher C.. Thompson, MD, MSc2, Pichamol Jirapinyo, MD, MPH3. P3889 - Modified Endoscopic Submucosal Dissection (ESD) With Suturing for the Treatment of Gastro-Gastric Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brigham and Women's Hospital, Boston, MA; 2Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 3Brigham and Women's Hospital, Boston, MA
Introduction: Gastro-gastric fistulae (GGF) may occur in upto 6% of patients following Roux-en-Y gastric bypass (RYGB). Various endoscopic approaches to treat GGF have been described including endoscopic suturing. Nevertheless, the efficacy of suturing at treating GGF, especially for those with a diameter of >1 cm, remains suboptimal. Here, we present a case of a large GGF treated with a combined endoscopic submucosal dissection (ESD) with suturing technique, aimed at improving efficacy and durability results.
Case Description/Methods: A 53-year-old woman with a history of open Roux-en-Y gastric bypass in 2003 status post endoscopic revision of RYGB via a plication technique (i.e. ROSE procedure) in 2021, complicated by gastrojejunal anastomosis (GJA) stenosis treated successfully with a balloon dilation, who presented with reflux and weight regain. An upper gastrointestinal study revealed a GGF. On an endoscopy, 2 GGF were seen on the left side of the pouch measuring 12 mm and 16 mm in diameter. Given the large sizes of both GGFs, the decision was made to close them with a combined ESD with suturing technique. First, ESD was performed around the GGF to prepare the tissue prior to endoscopic suturing. Specifically, mucosal incision was performed circumferentially around the GJA using an injection knife. The dissected area was then trimmed to widen and expose the submucosal and/or muscular layer using the same injection knife. Argon plasma coagulation was then performed on the inner and outer rims of the dissected area. Suturing was then performed using a running suture pattern by placing stitches from the inside of the GGF through the exposed submucosal/muscular layer to close the GGF. Once the first GGF was closed, the same steps were repeated to close the second, distal GGF (Video). At the end of the procedure, both GGFs were closed successfully. There were no intra or post-procedural adverse events. At the 2-month follow-up, her weight decreased from 208 to 194 lbs, representing a 6.7% TWL. She reported resolution of reflux symptoms and was able to discontinue a proton pump inhibitor. A follow-up upper gastrointestinal study confirmed successful closure of both GGFs.
Discussion: Combining ESD with suturing is technically feasible and effective technique at treating GGF in patients with RYGB. Further studies are warranted to assess the durability of this novel technique.
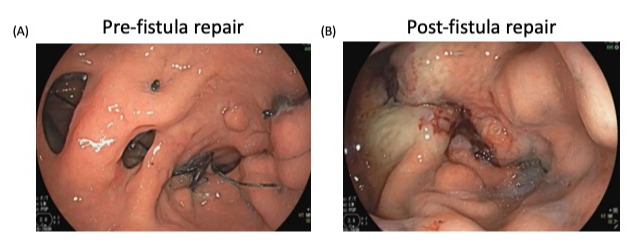
Figure: Figure 1: Pre-Fistula Repair (A); Post-Fistula Repair (B)
Disclosures:
Noppachai Siranart indicated no relevant financial relationships.
Christopher Thompson: Apollo Endosurgery – Consultant, Grant/Research Support. Bariendo – Consultant, Founder, Owner/Ownership Interest. Boston Scientific – Consultant, Grant/Research Support. Endoquest Robotics – Advisory Committee/Board Member, Consultant, Grant/Research Support. Endosim – Royalties. Enterasense Ltd. – Advisory Committee/Board Member, Consultant, Founder, Owner/Ownership Interest, Stock Options. EnVision Endoscopy – Advisory Committee/Board Member, Consultant, Founder, Owner/Ownership Interest, Stock Options. ERBE – Grant/Research Support. Fractyl – Consultant, Grant/Research Support, Stock Options. Fujifilm – Grant/Research Support. GI Dynamics – Consultant, Grant/Research Support. GI Windows – Advisory Committee/Board Member, Consultant, Founder, Owner/Ownership Interest, Royalties, Stock Options. Lumendi – Grant/Research Support. Medtronic – Advisory Committee/Board Member, Consultant. Olympus – Consultant, Grant/Research Support. USGI Medical – Advisory Committee/Board Member, Consultant, Grant/Research Support. Xenter – Advisory Committee/Board Member, Consultant.
Pichamol Jirapinyo: Apollo Endosurgery – Consultant, Grant/Research Support. Bariendo – Advisory Committee/Board Member, Consultant, Owner/Ownership Interest. Boston Scientific – Consultant, Grant/Research Support. Cook Medical – Consultant. Endosim – Royalties. ERBE – Consultant. Fractyl – Consultant, Grant/Research Support. GI Dynamics – Consultant, Grant/Research Support. Madrigal – Consultant. Spatz – Consultant. USGI Medical – Consultant, Grant/Research Support.
Noppachai Siranart, MD1, Christopher C.. Thompson, MD, MSc2, Pichamol Jirapinyo, MD, MPH3. P3889 - Modified Endoscopic Submucosal Dissection (ESD) With Suturing for the Treatment of Gastro-Gastric Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
