Tuesday Poster Session
Category: Endoscopy Video Forum
P3893 - Centering and Anchoring Approach to Endoscopically Manage Non-Healing PEG Site Fistula
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mayank Goyal, MBBS
Mayo Clinic
Rochester, MN
Presenting Author(s)
Mayank Goyal, MBBS1, Ashwariya Ohri, MBBS1, Khushboo Gala, MBBS2, Anmol Bains, MBBS1, Navtej Buttar, MD1
1Mayo Clinic, Rochester, MN; 2Mayo Clinic School of Graduate Medical Education, Rochester, MN
Introduction: Chronic non healing tube site after percutaneous endoscopic gastrostomy (PEG) tube removal is a rare and difficult to manage complication. Use of clips, sutures, gluing, banding, and coagulation techniques have been described as endoscopic therapeutic options for this indication, with limited success.
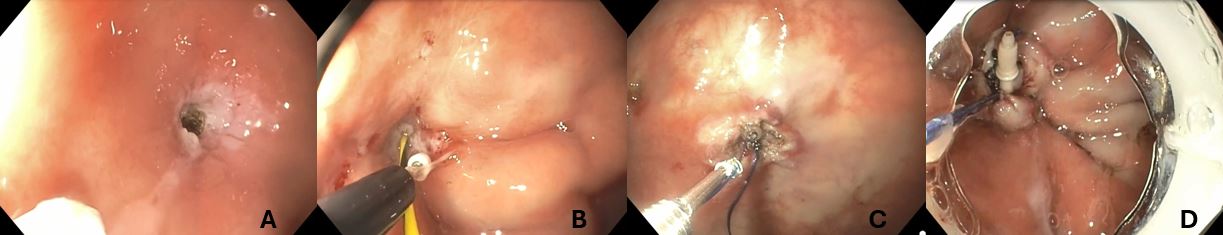
Case Description/Methods: We present a case of 23-year-old woman who had a significant past medical history of hypoplastic left heart syndrome status post heart transplant, and calcineurin inhibitor induced renal failure status post renal transplant (2011). She had been on enteral feeding via a PEG tube as child and then again for the last 5 years due to severe malnutrition. Her most recent tube was a 14 French, 3.5cm, ENFit AMT low profile tube, which was removed 5 weeks ago. She presented with significant mucoid and bilious discharge from the tube site, with a concern of non-healing site. On examination, the site was erythematous, and opening was approximately 6 mm in diameter. Given failure of healing by primary intention, we elected to proceed with endoscopic closure. On upper endoscopy, a 4mm gastrocutaneous fistula was visualized in the gastric body. We used a 4-step approach for the closure of the defect. Firstly, we de-epithelized the defect using argon plasma coagulation (Figure 1A). Secondly, we performed an escharectomy using a dual tip knife (Figure 1B) and avulsion forceps to remove the mucosa and submucosa. A 2.0 absorbable Vicryl suture was then brought with an “out-in” fashion through the gastrocutaneous fistula with help of snare to appropriately center the suture and close the cutaneous side. Subsequently, the endoscope loaded with x-tack and 2.0 polypropylene suture (Figure 1C). One suture was placed in a per string fashion to approximate the muscularis propria, with suture cinch used to approximate the defect. Lastly, an over-the-scope-clip was used to completely close the fistula site (Figure 1D). Stentfix was used due to its rounded design, this modified clip adapted well to the gastric anatomy. Patient tolerated the procedure well.
Discussion: Post-operatively, the patient was started on oral intake which she tolerated well. On 1 month follow up, the patient has been asymptomatic and maintaining her oral nutrition and healed gastrocutaneous fistula site.
Disclosures:
Mayank Goyal, MBBS1, Ashwariya Ohri, MBBS1, Khushboo Gala, MBBS2, Anmol Bains, MBBS1, Navtej Buttar, MD1. P3893 - Centering and Anchoring Approach to Endoscopically Manage Non-Healing PEG Site Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Mayo Clinic School of Graduate Medical Education, Rochester, MN
Introduction: Chronic non healing tube site after percutaneous endoscopic gastrostomy (PEG) tube removal is a rare and difficult to manage complication. Use of clips, sutures, gluing, banding, and coagulation techniques have been described as endoscopic therapeutic options for this indication, with limited success.
Case Description/Methods: We present a case of 23-year-old woman who had a significant past medical history of hypoplastic left heart syndrome status post heart transplant, and calcineurin inhibitor induced renal failure status post renal transplant (2011). She had been on enteral feeding via a PEG tube as child and then again for the last 5 years due to severe malnutrition. Her most recent tube was a 14 French, 3.5cm, ENFit AMT low profile tube, which was removed 5 weeks ago. She presented with significant mucoid and bilious discharge from the tube site, with a concern of non-healing site. On examination, the site was erythematous, and opening was approximately 6 mm in diameter. Given failure of healing by primary intention, we elected to proceed with endoscopic closure. On upper endoscopy, a 4mm gastrocutaneous fistula was visualized in the gastric body. We used a 4-step approach for the closure of the defect. Firstly, we de-epithelized the defect using argon plasma coagulation (Figure 1A). Secondly, we performed an escharectomy using a dual tip knife (Figure 1B) and avulsion forceps to remove the mucosa and submucosa. A 2.0 absorbable Vicryl suture was then brought with an “out-in” fashion through the gastrocutaneous fistula with help of snare to appropriately center the suture and close the cutaneous side. Subsequently, the endoscope loaded with x-tack and 2.0 polypropylene suture (Figure 1C). One suture was placed in a per string fashion to approximate the muscularis propria, with suture cinch used to approximate the defect. Lastly, an over-the-scope-clip was used to completely close the fistula site (Figure 1D). Stentfix was used due to its rounded design, this modified clip adapted well to the gastric anatomy. Patient tolerated the procedure well.
Discussion: Post-operatively, the patient was started on oral intake which she tolerated well. On 1 month follow up, the patient has been asymptomatic and maintaining her oral nutrition and healed gastrocutaneous fistula site.
Figure: A- de-epithelized using argon plasma coagulation
B- Escharectomy using dual tip knife\
C- use f X-tack and polypropylene suture
D- Stentfix OTSC to completely close the fistula
B- Escharectomy using dual tip knife\
C- use f X-tack and polypropylene suture
D- Stentfix OTSC to completely close the fistula
Disclosures:
Mayank Goyal indicated no relevant financial relationships.
Ashwariya Ohri indicated no relevant financial relationships.
Khushboo Gala indicated no relevant financial relationships.
Anmol Bains indicated no relevant financial relationships.
Navtej Buttar indicated no relevant financial relationships.
Mayank Goyal, MBBS1, Ashwariya Ohri, MBBS1, Khushboo Gala, MBBS2, Anmol Bains, MBBS1, Navtej Buttar, MD1. P3893 - Centering and Anchoring Approach to Endoscopically Manage Non-Healing PEG Site Fistula, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
