Tuesday Poster Session
Category: Colorectal Cancer Prevention
P3843 - Colorectal Cancer Trends and Metabolic Risk Factors: A Global Analysis and Future Projections to 2030
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MK
Meghana Kakarla, MD
Infirmary Health
durham, India
Presenting Author(s)
Meghana Kakarla, MD1, Bijay Mukesh Jeswani, MBBS2, Jo-Amadi Precious Oroma, MS3, Hafiza Amna Qadeer, MBBS4, Tirath Daishikbhai Patel, MS5, Ujwala Reddy Borra, MBBS6, Hairya Ajaykumar Lakhani, MBBS7
1Infirmary Health, Mobile, AL; 2GCS Medical College, Hospital & Research Centre, Ahmedabad, Gujarat, India; 3All Saints University School of Medicine, Roseau, Saint George, Dominica; 4Foundation University Medical College, Islamabad, Punjab, Pakistan; 5American University of Antigua, Osbourn, Saint John, Antigua and Barbuda; 6MediCiti Institute of Medical Sciences, Hyderabad, Telangana, India; 7SBKS Medical Institute and Research Center, Vadodara, Gujarat, India
Introduction: Colorectal cancer (CRC) is a major global health concern with high morbidity and mortality rates. Despite ongoing research and advancements in treatment, there remains a need to understand the complex interplay between CRC trends, the impact of metabolic risk factors, and future projections. This study aims to analyze current CRC trends, evaluate the impact of metabolic risk factors, and project future outcomes up to 2030.
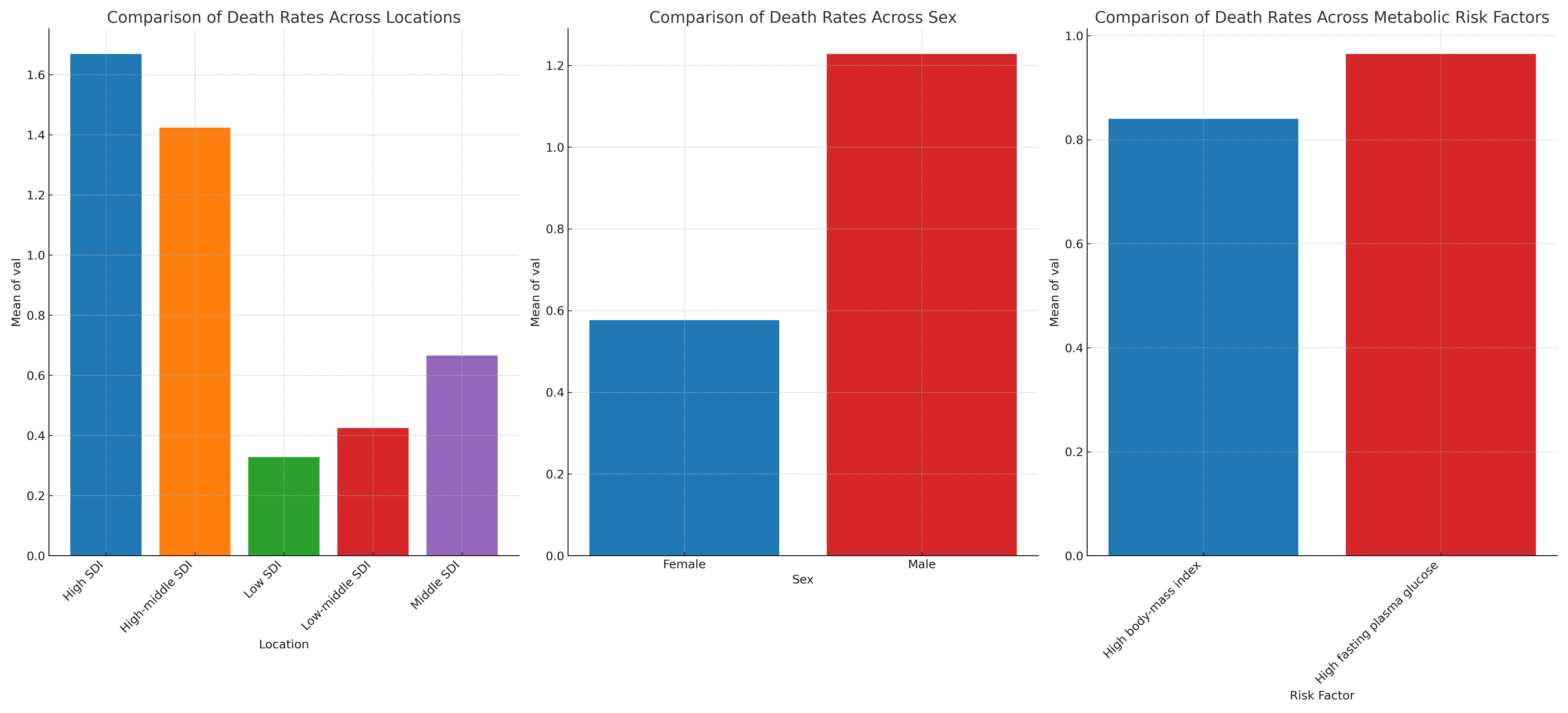
Methods: Data on age-standardized death and Disability-Adjusted Life Years (DALYs) for CRC were obtained from the Global Burden of Disease (GBD) study, covering 1990 to 2019. Linear regression analysis was utilized to identify trends and predict values up to 2030. Comparative analysis was conducted across different regions, sexes, and key metabolic risk factors, including obesity, diabetes, and hyperlipidemia. The estimated annual percentage change was calculated to quantify trends.
Results: From 1990 to 2019, CRC-related death rates decreased significantly, with a mean annual reduction of 1.5%. The linear regression model projects a 25% reduction in age-standardized death rates and a 30% reduction in DALY rates by 2030. Comparative analysis revealed regional disparities, with high-income regions achieving a 35% reduction in death rates, while low- and middle-income regions saw only a 10% reduction. Sex-based differences indicated that males had a 20% higher CRC death rate compared to females. Metabolic risk factors significantly impacted CRC rates, with obesity-related CRC cases increasing by 15% and diabetes-related cases by 10% over the study period.
Discussion: The declining trends in CRC-related deaths and DALYs suggest improvements in early detection, treatment, and prevention strategies. However, regional and sex-based disparities highlight the need for targeted public health interventions. The increasing impact of metabolic risk factors on CRC underscores the importance of addressing lifestyle and dietary factors in prevention programs. Efforts to reduce obesity and improve diabetes management are crucial for mitigating future CRC burdens. Colorectal cancer remains a major public health issue with evolving trends and significant future challenges. Proactive measures addressing metabolic risk factors and targeted interventions are essential to further reduce the global CRC burden by 2030. Continued research and policy efforts are necessary to sustain and enhance these positive trends.
Disclosures:
Meghana Kakarla, MD1, Bijay Mukesh Jeswani, MBBS2, Jo-Amadi Precious Oroma, MS3, Hafiza Amna Qadeer, MBBS4, Tirath Daishikbhai Patel, MS5, Ujwala Reddy Borra, MBBS6, Hairya Ajaykumar Lakhani, MBBS7. P3843 - Colorectal Cancer Trends and Metabolic Risk Factors: A Global Analysis and Future Projections to 2030, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Infirmary Health, Mobile, AL; 2GCS Medical College, Hospital & Research Centre, Ahmedabad, Gujarat, India; 3All Saints University School of Medicine, Roseau, Saint George, Dominica; 4Foundation University Medical College, Islamabad, Punjab, Pakistan; 5American University of Antigua, Osbourn, Saint John, Antigua and Barbuda; 6MediCiti Institute of Medical Sciences, Hyderabad, Telangana, India; 7SBKS Medical Institute and Research Center, Vadodara, Gujarat, India
Introduction: Colorectal cancer (CRC) is a major global health concern with high morbidity and mortality rates. Despite ongoing research and advancements in treatment, there remains a need to understand the complex interplay between CRC trends, the impact of metabolic risk factors, and future projections. This study aims to analyze current CRC trends, evaluate the impact of metabolic risk factors, and project future outcomes up to 2030.
Methods: Data on age-standardized death and Disability-Adjusted Life Years (DALYs) for CRC were obtained from the Global Burden of Disease (GBD) study, covering 1990 to 2019. Linear regression analysis was utilized to identify trends and predict values up to 2030. Comparative analysis was conducted across different regions, sexes, and key metabolic risk factors, including obesity, diabetes, and hyperlipidemia. The estimated annual percentage change was calculated to quantify trends.
Results: From 1990 to 2019, CRC-related death rates decreased significantly, with a mean annual reduction of 1.5%. The linear regression model projects a 25% reduction in age-standardized death rates and a 30% reduction in DALY rates by 2030. Comparative analysis revealed regional disparities, with high-income regions achieving a 35% reduction in death rates, while low- and middle-income regions saw only a 10% reduction. Sex-based differences indicated that males had a 20% higher CRC death rate compared to females. Metabolic risk factors significantly impacted CRC rates, with obesity-related CRC cases increasing by 15% and diabetes-related cases by 10% over the study period.
Discussion: The declining trends in CRC-related deaths and DALYs suggest improvements in early detection, treatment, and prevention strategies. However, regional and sex-based disparities highlight the need for targeted public health interventions. The increasing impact of metabolic risk factors on CRC underscores the importance of addressing lifestyle and dietary factors in prevention programs. Efforts to reduce obesity and improve diabetes management are crucial for mitigating future CRC burdens. Colorectal cancer remains a major public health issue with evolving trends and significant future challenges. Proactive measures addressing metabolic risk factors and targeted interventions are essential to further reduce the global CRC burden by 2030. Continued research and policy efforts are necessary to sustain and enhance these positive trends.
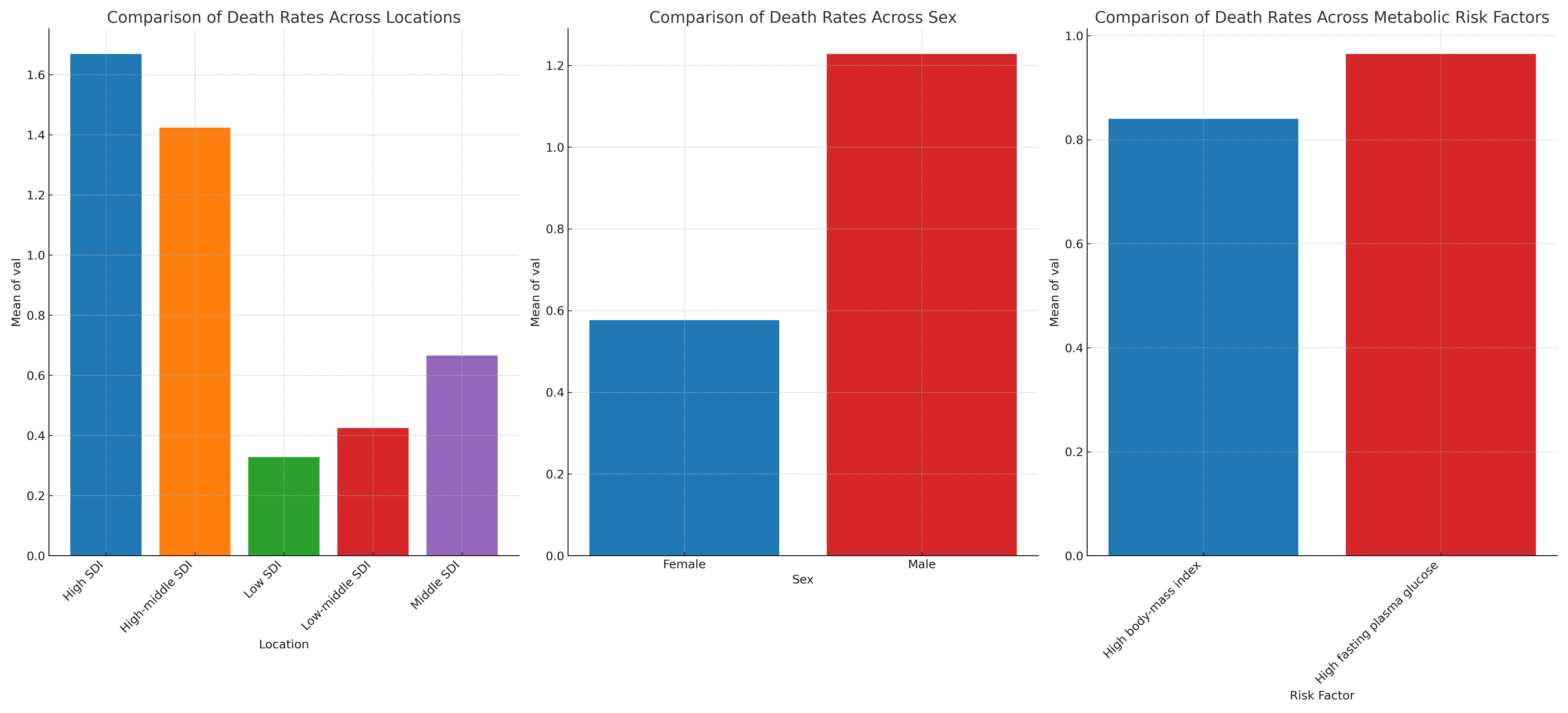
Figure: Trends and Projections in Colorectal Cancer Mortality and Disability-Adjusted Life Years (1990-2030), with Comparison Across Locations, Sex, and Metabolic Risk Factors
Disclosures:
Meghana Kakarla indicated no relevant financial relationships.
Bijay Mukesh Jeswani indicated no relevant financial relationships.
Jo-Amadi Precious Oroma indicated no relevant financial relationships.
Hafiza Amna Qadeer indicated no relevant financial relationships.
Tirath Daishikbhai Patel indicated no relevant financial relationships.
Ujwala Reddy Borra indicated no relevant financial relationships.
Hairya Ajaykumar Lakhani indicated no relevant financial relationships.
Meghana Kakarla, MD1, Bijay Mukesh Jeswani, MBBS2, Jo-Amadi Precious Oroma, MS3, Hafiza Amna Qadeer, MBBS4, Tirath Daishikbhai Patel, MS5, Ujwala Reddy Borra, MBBS6, Hairya Ajaykumar Lakhani, MBBS7. P3843 - Colorectal Cancer Trends and Metabolic Risk Factors: A Global Analysis and Future Projections to 2030, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
