Tuesday Poster Session
Category: Colon
P3779 - Antipsychotic-Induced Bowel Crisis: Rare Case of Clozapine-Triggered Ischemic Colitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Guneet Sidhu, MD
University of North Dakota
Fargo, ND
Presenting Author(s)
Guneet Sidhu, MD1, John Bassett, MD, FACG2, Rajendra Potluri, MD3
1University of North Dakota, Fargo, ND; 2Sanford Health, Fargo, ND; 3Sanford Medical Center, Fargo, ND
Introduction: Clozapine, an atypical antipsychotic, is primarily utilized for treatment-resistant schizophrenia due to its efficacy in reducing symptoms when other antipsychotics fail. Despite its clinical benefits, clozapine is associated with a spectrum of adverse effects, among which gastrointestinal complications, including colitis, are significant yet underrecognized.
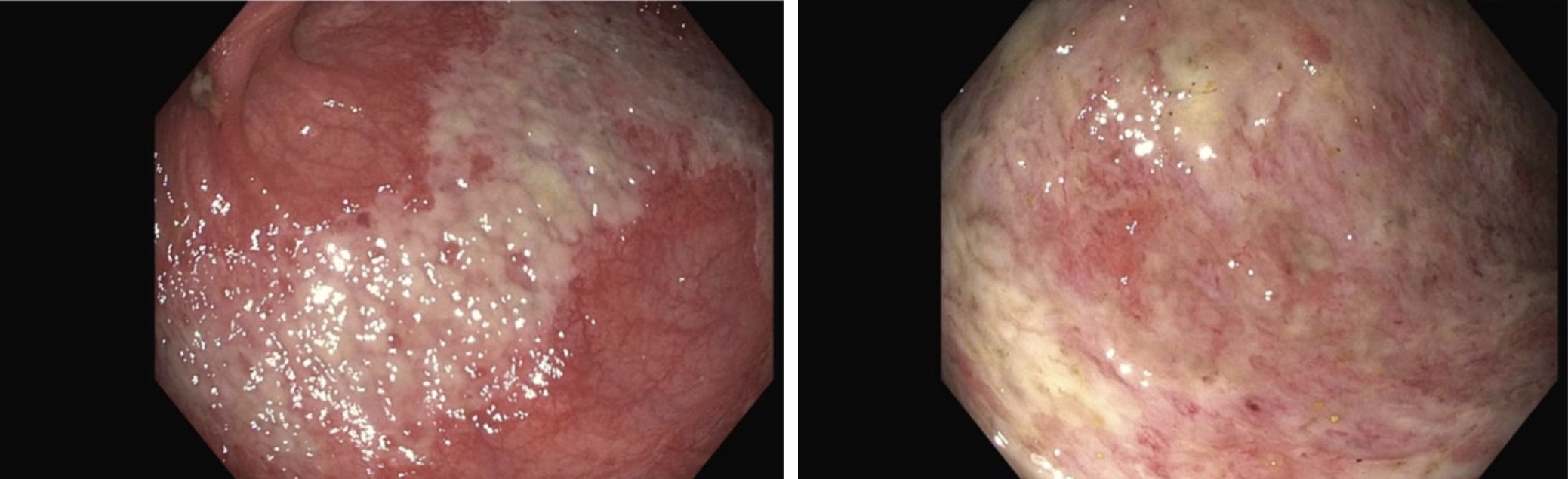
Case Description/Methods: 73 Y female presented with generalized weakness and abdominal pain of two days. She had been experiencing chronic constipation. Patient was hypotensive, elevated lactic acid, leukocytosis, and an increased CRP. She received 2L boluses of fluids and was started on Rocephin and Flagyl. Tests for C. difficile and other enteric pathogens were negative. CT scan revealed colitis. The patient had a history of treatment-resistant schizophrenia and psychosis that only responded to clozapine. GI and psychiatry consultations were obtained. Psychiatry recommended discontinuing all antipsychotics including clozapine, while GI advised colonoscopy, which showed non-bleeding ulcerated mucosa consistent with ischemic colitis. Despite these interventions, the patient's abdominal pain worsened. A follow-up CT scan indicated bowel dilation with no clear transition point. NG tube for bowel decompression was placed which yielded 2.5L of output, resulting in pain and distension improvement. Patient suddenly experienced increasing abdominal pain, raising concerns of toxic megacolon. KUB indicated increased colonic dilation from 6.7 cm to 7.9 cm. A subsequent colonoscopy continued to show non-bleeding ulcerated mucosa over 40 cm length. Biopsies confirmed colonic mucosa with erosion, fibrinopurulent exudate, and ischemic changes. CRP levels began to decline. Psychiatry ceased congentin to mitigate the risk of megacolon and initiated propranolol for tardive dyskinesia. The patient improved off clozapine and bowel rest.
Discussion: Clozapine-induced gastrointestinal hypomotility is a severe and potentially life-threatening complication. The anticholinergic and antiserotonergic properties of clozapine significantly impair gastrointestinal motility. In this case, the patient's chronic constipation was exacerbated by clozapine contributing to the development of ischemic colitis. Management of clozapine-induced colitis involves discontinuation of the offending agent, supportive care and bowel decompression. The co-prescription of laxatives and routine counseling on bowel health for patients on clozapine is important
Disclosures:
Guneet Sidhu, MD1, John Bassett, MD, FACG2, Rajendra Potluri, MD3. P3779 - Antipsychotic-Induced Bowel Crisis: Rare Case of Clozapine-Triggered Ischemic Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Dakota, Fargo, ND; 2Sanford Health, Fargo, ND; 3Sanford Medical Center, Fargo, ND
Introduction: Clozapine, an atypical antipsychotic, is primarily utilized for treatment-resistant schizophrenia due to its efficacy in reducing symptoms when other antipsychotics fail. Despite its clinical benefits, clozapine is associated with a spectrum of adverse effects, among which gastrointestinal complications, including colitis, are significant yet underrecognized.
Case Description/Methods: 73 Y female presented with generalized weakness and abdominal pain of two days. She had been experiencing chronic constipation. Patient was hypotensive, elevated lactic acid, leukocytosis, and an increased CRP. She received 2L boluses of fluids and was started on Rocephin and Flagyl. Tests for C. difficile and other enteric pathogens were negative. CT scan revealed colitis. The patient had a history of treatment-resistant schizophrenia and psychosis that only responded to clozapine. GI and psychiatry consultations were obtained. Psychiatry recommended discontinuing all antipsychotics including clozapine, while GI advised colonoscopy, which showed non-bleeding ulcerated mucosa consistent with ischemic colitis. Despite these interventions, the patient's abdominal pain worsened. A follow-up CT scan indicated bowel dilation with no clear transition point. NG tube for bowel decompression was placed which yielded 2.5L of output, resulting in pain and distension improvement. Patient suddenly experienced increasing abdominal pain, raising concerns of toxic megacolon. KUB indicated increased colonic dilation from 6.7 cm to 7.9 cm. A subsequent colonoscopy continued to show non-bleeding ulcerated mucosa over 40 cm length. Biopsies confirmed colonic mucosa with erosion, fibrinopurulent exudate, and ischemic changes. CRP levels began to decline. Psychiatry ceased congentin to mitigate the risk of megacolon and initiated propranolol for tardive dyskinesia. The patient improved off clozapine and bowel rest.
Discussion: Clozapine-induced gastrointestinal hypomotility is a severe and potentially life-threatening complication. The anticholinergic and antiserotonergic properties of clozapine significantly impair gastrointestinal motility. In this case, the patient's chronic constipation was exacerbated by clozapine contributing to the development of ischemic colitis. Management of clozapine-induced colitis involves discontinuation of the offending agent, supportive care and bowel decompression. The co-prescription of laxatives and routine counseling on bowel health for patients on clozapine is important
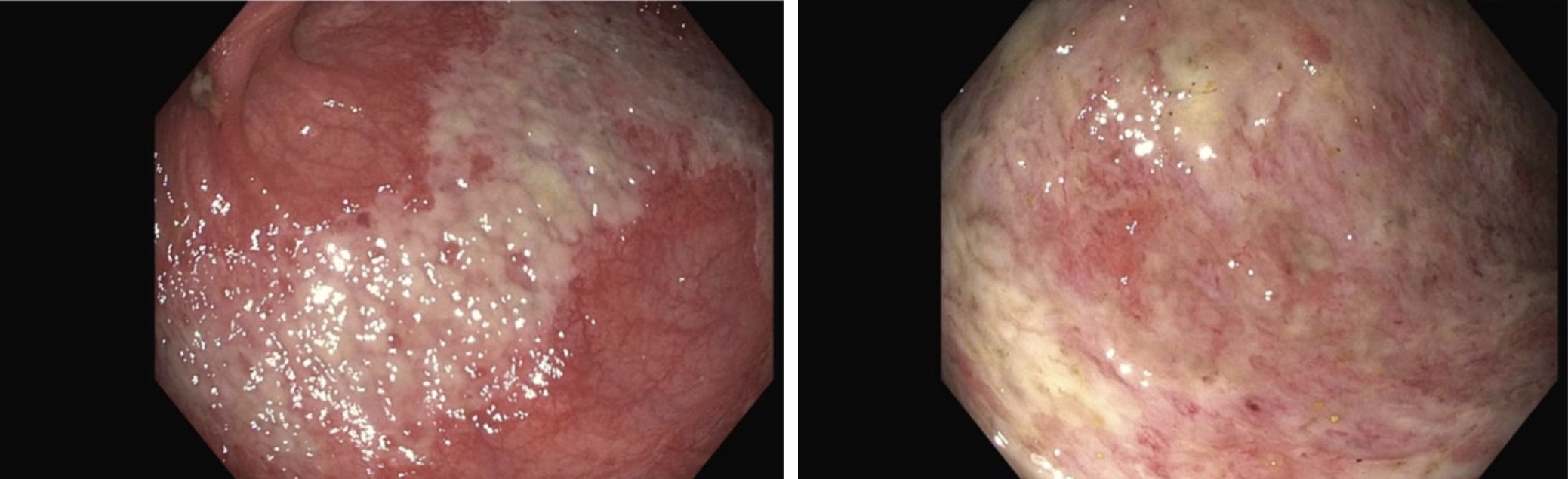
Figure: Area of necrosis in the sigmoid colon
Disclosures:
Guneet Sidhu indicated no relevant financial relationships.
John Bassett indicated no relevant financial relationships.
Rajendra Potluri indicated no relevant financial relationships.
Guneet Sidhu, MD1, John Bassett, MD, FACG2, Rajendra Potluri, MD3. P3779 - Antipsychotic-Induced Bowel Crisis: Rare Case of Clozapine-Triggered Ischemic Colitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
