Tuesday Poster Session
Category: Colon
P3709 - Endoscopic Ultrasound-Guided Diagnosis of A Rare Cecal/Appendiceal Subepithelial Lesion: An Intramural Pseudocyst
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Harneet Sangha, BS
Washington State University Elson S. Floyd College of Medicine
Spokane, WA
Presenting Author(s)
Award: Presidential Poster Award
Harneet Sangha, BS1, Tavishi Girotra, MBBS2, Shreya Chopra, MBBS2, Navansh Johnson, 2, Anusha Singhania, MBBS2, Mohit Girotra, MD1, Christopher Carlson, MD2
1Washington State University Elson S. Floyd College of Medicine, Spokane, WA; 2Digestive Health Institute, Swedish Medical Center, Seattle, WA
Introduction: Intramural pseudocysts are extremely rare, with only a handful of reports in literature. The exact mechanism is unclear, they are speculated to form in response to inflammation/infection, but mostly seen after acute/chronic pancreatitis wherein, leakage of digestive enzymes results in a localized fluid collection within the bowel wall. When reported, they are usually in the upper GI tract, and present with non-specific abdominal symptoms.
Endoscopic ultrasound (EUS) plays a crucial role in evaluation of GI subepithelial lesions, as well as for evaluation/management of fluid collections around the GI tract. We report a unique case cecal/appendiceal intramural pseudocyst, evaluated with EUS.
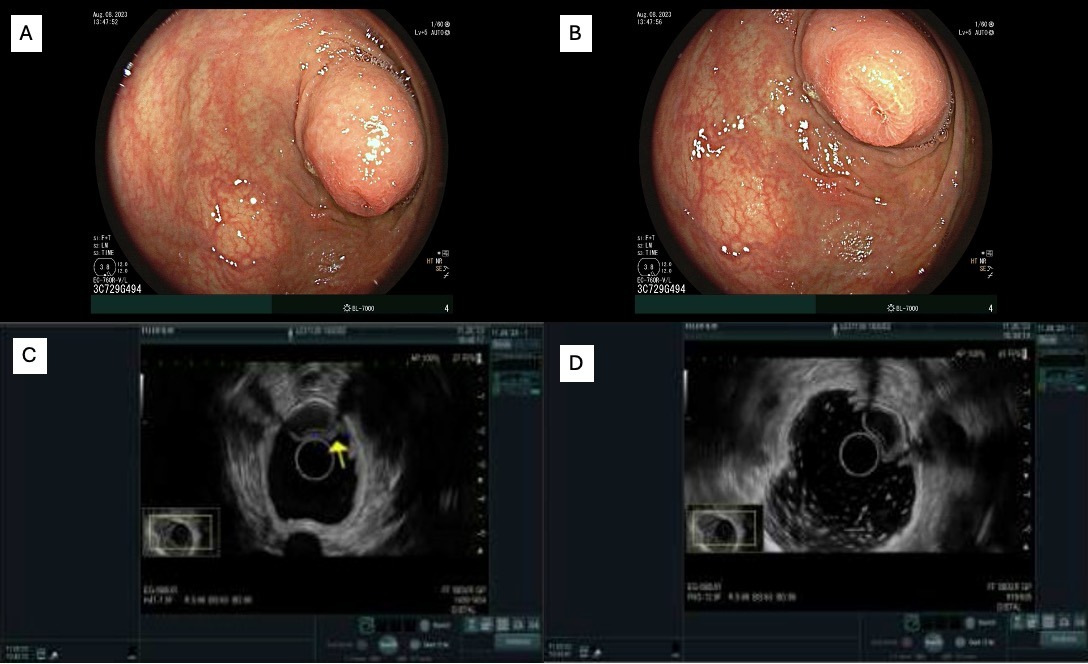
Case Description/Methods: A 59-year-old man with myeloproliferative disease and associated Janus-Kinase2 (JAK2) mutation, polycythemia vera, family history of lymphoma/leukemia and chronic consumption of 1-2 alcoholic drinks a week underwent colonoscopy for iron deficiency, which incidentally noted a subepithelial nodule at the appendiceal orifice.
Patient was referred for EUS, which confirmed a 10.8x16.6mm moderately heterogeneous hypoechoic lesion without shadowing at the appendiceal orifice, appearing consistent with a mucocele. Hypoechoic area was inside of the interface layer and didn’t seem to arise from any particular layer. Cecal nodule surface biopsy revealed colonic mucosa without any significant histopathologic abnormality, infectious agents, or features of microscopic colitis, and was negative for dysplasia.
With concern for mucocele, patient underwent appendectomy, and surgical pathology confirmed intramural pseudocyst, without dysplasia.
Discussion: GI intramural pseudocysts often present with non-specific symptoms such as abdominal pain and changes in bowel habits, and treatment varies from observation to endoscopic drainage or surgical intervention.
The exploration of appendiceal nodules is crucial due to their potential to be malignant such as mucocele or carcinoid, if left untreated. Mucoceles are cystic lesions that can arise from obstruction and dilation of the appendiceal lumen, leading to the accumulation of mucus. EUS is valuable in assessing the characteristics of these subepithelial nodules, aiding in the distinction of their contents, and guiding clinical management.
Our unique case, does not have a precedence in available EUS literature, highlights the importance of maintaining intramural pseudocyst as a differential on EUS, when encountering mucocele like lesions.
Disclosures:
Harneet Sangha, BS1, Tavishi Girotra, MBBS2, Shreya Chopra, MBBS2, Navansh Johnson, 2, Anusha Singhania, MBBS2, Mohit Girotra, MD1, Christopher Carlson, MD2. P3709 - Endoscopic Ultrasound-Guided Diagnosis of A Rare Cecal/Appendiceal Subepithelial Lesion: An Intramural Pseudocyst, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Harneet Sangha, BS1, Tavishi Girotra, MBBS2, Shreya Chopra, MBBS2, Navansh Johnson, 2, Anusha Singhania, MBBS2, Mohit Girotra, MD1, Christopher Carlson, MD2
1Washington State University Elson S. Floyd College of Medicine, Spokane, WA; 2Digestive Health Institute, Swedish Medical Center, Seattle, WA
Introduction: Intramural pseudocysts are extremely rare, with only a handful of reports in literature. The exact mechanism is unclear, they are speculated to form in response to inflammation/infection, but mostly seen after acute/chronic pancreatitis wherein, leakage of digestive enzymes results in a localized fluid collection within the bowel wall. When reported, they are usually in the upper GI tract, and present with non-specific abdominal symptoms.
Endoscopic ultrasound (EUS) plays a crucial role in evaluation of GI subepithelial lesions, as well as for evaluation/management of fluid collections around the GI tract. We report a unique case cecal/appendiceal intramural pseudocyst, evaluated with EUS.
Case Description/Methods: A 59-year-old man with myeloproliferative disease and associated Janus-Kinase2 (JAK2) mutation, polycythemia vera, family history of lymphoma/leukemia and chronic consumption of 1-2 alcoholic drinks a week underwent colonoscopy for iron deficiency, which incidentally noted a subepithelial nodule at the appendiceal orifice.
Patient was referred for EUS, which confirmed a 10.8x16.6mm moderately heterogeneous hypoechoic lesion without shadowing at the appendiceal orifice, appearing consistent with a mucocele. Hypoechoic area was inside of the interface layer and didn’t seem to arise from any particular layer. Cecal nodule surface biopsy revealed colonic mucosa without any significant histopathologic abnormality, infectious agents, or features of microscopic colitis, and was negative for dysplasia.
With concern for mucocele, patient underwent appendectomy, and surgical pathology confirmed intramural pseudocyst, without dysplasia.
Discussion: GI intramural pseudocysts often present with non-specific symptoms such as abdominal pain and changes in bowel habits, and treatment varies from observation to endoscopic drainage or surgical intervention.
The exploration of appendiceal nodules is crucial due to their potential to be malignant such as mucocele or carcinoid, if left untreated. Mucoceles are cystic lesions that can arise from obstruction and dilation of the appendiceal lumen, leading to the accumulation of mucus. EUS is valuable in assessing the characteristics of these subepithelial nodules, aiding in the distinction of their contents, and guiding clinical management.
Our unique case, does not have a precedence in available EUS literature, highlights the importance of maintaining intramural pseudocyst as a differential on EUS, when encountering mucocele like lesions.
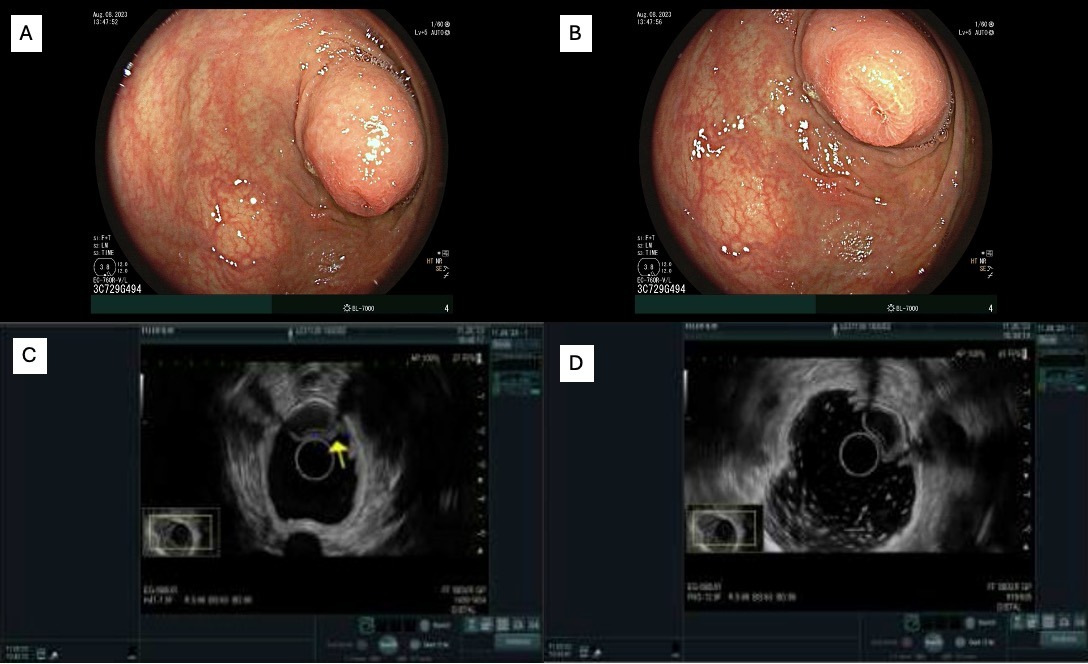
Figure: A and B: Endoscopy of 16 mm subepithelial nodule at the appendiceal orifice;
C and D: EUS showing a 10.8x16.6 moderately heterogeneous hypoechoic area at the appendiceal orifice.
C and D: EUS showing a 10.8x16.6 moderately heterogeneous hypoechoic area at the appendiceal orifice.
Disclosures:
Harneet Sangha indicated no relevant financial relationships.
Tavishi Girotra indicated no relevant financial relationships.
Shreya Chopra indicated no relevant financial relationships.
Navansh Johnson indicated no relevant financial relationships.
Anusha Singhania indicated no relevant financial relationships.
Mohit Girotra indicated no relevant financial relationships.
Christopher Carlson indicated no relevant financial relationships.
Harneet Sangha, BS1, Tavishi Girotra, MBBS2, Shreya Chopra, MBBS2, Navansh Johnson, 2, Anusha Singhania, MBBS2, Mohit Girotra, MD1, Christopher Carlson, MD2. P3709 - Endoscopic Ultrasound-Guided Diagnosis of A Rare Cecal/Appendiceal Subepithelial Lesion: An Intramural Pseudocyst, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

