Tuesday Poster Session
Category: Colon
P3677 - A One in a Million Case of Gastrointestinal Histiocytic Sarcoma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- HS
Hillary C. Smalley, DO
Naval Medical Center San Diego
San Diego, CA
Presenting Author(s)
Hillary C. Smalley, DO1, Thomas Mellor, DO2, Daniel Jack, MD3
1Naval Medical Center San Diego, San Diego, CA; 2Naval Hospital Bremerton, Bremerton, WA; 3Madigan Army Medical Center, Joint Base Lewis-McChord, WA
Introduction:
We present a highly unusual diagnosis of malignant histiocytic sarcoma (HS) of gastrointestinal origin necessitating a multidisciplinary approach given the rarity and lack of standardized treatment regimens.
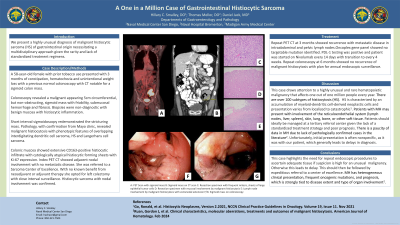
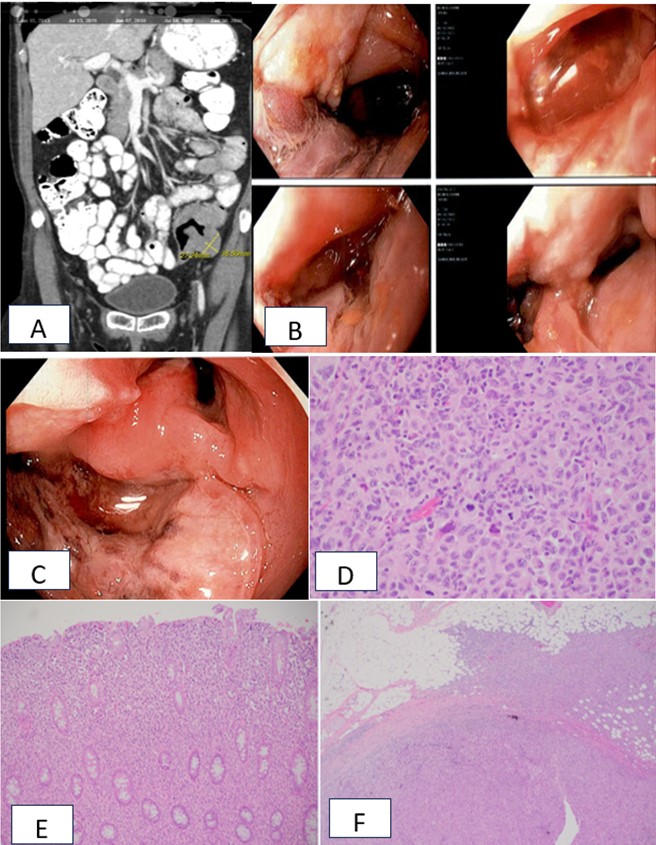
Case Description/Methods: A 58-year-old female with prior tobacco use presented with 3 months of constipation, hematochezia and unintentional weight loss with a previous normal colonoscopy with CT notable for a sigmoid colon mass. Colonoscopy revealed a malignant appearing 5cm circumferential, but non-obstructing, sigmoid mass with friability, submucosal hemorrhage and fibrosis. Biopsies were non-diagnostic with benign mucosa with histiocytic inflammation. Short interval sigmoidoscopy redemonstrated the stricturing mass. Pathology, with confirmation from Mayo clinic, revealed malignant histiocytosis with phenotypic features of overlapping interdigitating dendritic cell sarcoma, HS and Langerhans cell sarcoma. Colonic mucosa showed extensive CD163-positive histiocytic infiltrate with cytologically atypical histiocytic forming sheets with Ki-67 expression. Index PET CT showed adjacent nodal involvement with no metastatic disease. She was referred to a Sarcoma Center of Excellence. With no known benefit from neoadjuvant or adjuvant therapy she opted for left colectomy with close interval surveillance. Histiocytic sarcoma with nodal involvement was confirmed. Repeat PET CT at 3 months showed recurrence with metastatic disease in intraabdominal and pelvic lymph nodes. Oncoplex gene panel showed no targetable mutation identified. PDL-1 testing was positive and patient was started on Nivolumab every 14 days with transition to every 4 weeks. Repeat colonoscopy at 6 months showed no recurrence of malignant histiocytosis with plan for annual endoscopic surveillance.
Discussion: This case draws attention to a highly unusual and rare hematopoietic malignancy that affects one out of one million people every year. HS is characterized by an accumulation of myeloid-dendritic cell-derived neoplastic cells and presentation varies from localized to catastrophic. Patients should ideally be managed at a tertiary referral center given the lack of a standardized treatment strategy and poor prognosis. Unfortunately, initial presentation is often nonspecific, as it was with our patient, which generally leads to delays in diagnosis and highlights the need for repeat endoscopic procedures to ascertain adequate tissue if suspicion is high for malignancy followed by expeditious referral to a center of excellence.
Disclosures:
Hillary C. Smalley, DO1, Thomas Mellor, DO2, Daniel Jack, MD3. P3677 - A One in a Million Case of Gastrointestinal Histiocytic Sarcoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Naval Medical Center San Diego, San Diego, CA; 2Naval Hospital Bremerton, Bremerton, WA; 3Madigan Army Medical Center, Joint Base Lewis-McChord, WA
Introduction:
We present a highly unusual diagnosis of malignant histiocytic sarcoma (HS) of gastrointestinal origin necessitating a multidisciplinary approach given the rarity and lack of standardized treatment regimens.
Case Description/Methods: A 58-year-old female with prior tobacco use presented with 3 months of constipation, hematochezia and unintentional weight loss with a previous normal colonoscopy with CT notable for a sigmoid colon mass. Colonoscopy revealed a malignant appearing 5cm circumferential, but non-obstructing, sigmoid mass with friability, submucosal hemorrhage and fibrosis. Biopsies were non-diagnostic with benign mucosa with histiocytic inflammation. Short interval sigmoidoscopy redemonstrated the stricturing mass. Pathology, with confirmation from Mayo clinic, revealed malignant histiocytosis with phenotypic features of overlapping interdigitating dendritic cell sarcoma, HS and Langerhans cell sarcoma. Colonic mucosa showed extensive CD163-positive histiocytic infiltrate with cytologically atypical histiocytic forming sheets with Ki-67 expression. Index PET CT showed adjacent nodal involvement with no metastatic disease. She was referred to a Sarcoma Center of Excellence. With no known benefit from neoadjuvant or adjuvant therapy she opted for left colectomy with close interval surveillance. Histiocytic sarcoma with nodal involvement was confirmed. Repeat PET CT at 3 months showed recurrence with metastatic disease in intraabdominal and pelvic lymph nodes. Oncoplex gene panel showed no targetable mutation identified. PDL-1 testing was positive and patient was started on Nivolumab every 14 days with transition to every 4 weeks. Repeat colonoscopy at 6 months showed no recurrence of malignant histiocytosis with plan for annual endoscopic surveillance.
Discussion: This case draws attention to a highly unusual and rare hematopoietic malignancy that affects one out of one million people every year. HS is characterized by an accumulation of myeloid-dendritic cell-derived neoplastic cells and presentation varies from localized to catastrophic. Patients should ideally be managed at a tertiary referral center given the lack of a standardized treatment strategy and poor prognosis. Unfortunately, initial presentation is often nonspecific, as it was with our patient, which generally leads to delays in diagnosis and highlights the need for repeat endoscopic procedures to ascertain adequate tissue if suspicion is high for malignancy followed by expeditious referral to a center of excellence.
Figure: A: PET Scan with sigmoid mass
B: Sigmoid mass on colonoscopy
C: Sigmoid mass on flexible sigmoidoscopy
D. Resection specimen with frequent mitosis, sheets of large epithelial tumor cells
E: Resection specimen with mucosal involvement by malignant histiocytosis
F: Lymph node involvement by malignant histiocytosis with extranodal extension into the surrounding adipose tissue
B: Sigmoid mass on colonoscopy
C: Sigmoid mass on flexible sigmoidoscopy
D. Resection specimen with frequent mitosis, sheets of large epithelial tumor cells
E: Resection specimen with mucosal involvement by malignant histiocytosis
F: Lymph node involvement by malignant histiocytosis with extranodal extension into the surrounding adipose tissue
Disclosures:
Hillary Smalley indicated no relevant financial relationships.
Thomas Mellor indicated no relevant financial relationships.
Daniel Jack indicated no relevant financial relationships.
Hillary C. Smalley, DO1, Thomas Mellor, DO2, Daniel Jack, MD3. P3677 - A One in a Million Case of Gastrointestinal Histiocytic Sarcoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
