Tuesday Poster Session
Category: Biliary/Pancreas
P3582 - Hepatic Arteriobiliary Fistula Causing Massive Hemobilia: Successful Treatment With Coil Embolization
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Aishwarya Thakurdesai, MBBS
University of Louisville School of Medicine
Louisville, KY
Presenting Author(s)
Aishwarya Thakurdesai, MBBS, Bryan Glaenzer, MD, Ashwani Singal, MD, MS, Dipendra Parajuli, MD
University of Louisville School of Medicine, Louisville, KY
Introduction: Hemobilia, or the presence of blood in the biliary tree, is an important cause of gastrointestinal bleeding. It is a frequent complication of percutaneous transhepatic biliary drainage (PTBD). Most of these episodes are self-limited, however, in less than 5% of cases, hemobilia is clinically significant, and may require urgent intervention. Prompt diagnosis of major hemobilia causing hemodynamic instability can be challenging. We present a case of massive hemobilia due to hepatic arteriobiliary fistula formation after PTBD placement.
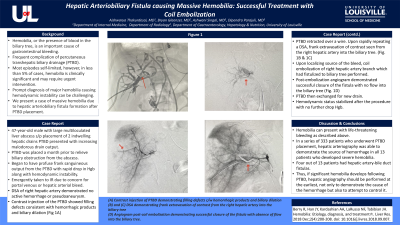
Case Description/Methods: A 47-year-old male with a large multiloculated liver abscess who had undergone placement of 2 indwelling hepatic drains and a percutaneous transhepatic biliary drain (PTBD) presented with increasing malodorous drain output. The PTBD was placed a month prior to relieve biliary obstruction from the abscess. During his clinical course, he began to have profuse frank sanguineous output from the PTBD with a rapid drop in hemoglobin along with hemodynamic instability. He was emergently taken to Interventional Radiology due to concern for a portal venous or hepatic arterial bleed. A digital subtraction angiogram (DSA) of the right hepatic artery demonstrated no active hemorrhage or pseudoaneurysm. Contrast injection of the PTBD showed filling defects consistent with hemorrhagic products and biliary dilation. The PTBD was retracted over a wire. Upon rapidly repeating a DSA, frank extravasation of contrast was seen from the right hepatic artery into the biliary tree. Upon localizing the source of the bleed, coil embolization of the branch of the right hepatic artery which had fistulized to the biliary tree was carried out. Post-embolization angiogram demonstrated successful closure of the fistula with no flow into the biliary tree. The PTBD was then exchanged for a new drain. The patient’s hemodynamic status stabilized after the procedure with no further drop in hemoglobin.
Discussion: Hemobilia can present with life-threatening bleeding as described above. In a series of 333 patients who underwent PTBD placement, hepatic arteriography was able to demonstrate the source of hemorrhage in all 13 patients who developed severe hemobilia. Four out of 13 patients had hepatic artery-bile duct fistulas. Thus, if significant hemobilia develops following PTBD, hepatic angiography should be performed at the earliest, not only to demonstrate the cause of the hemorrhage but also to attempt to control it.

Disclosures:
Aishwarya Thakurdesai, MBBS, Bryan Glaenzer, MD, Ashwani Singal, MD, MS, Dipendra Parajuli, MD. P3582 - Hepatic Arteriobiliary Fistula Causing Massive Hemobilia: Successful Treatment With Coil Embolization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Louisville School of Medicine, Louisville, KY
Introduction: Hemobilia, or the presence of blood in the biliary tree, is an important cause of gastrointestinal bleeding. It is a frequent complication of percutaneous transhepatic biliary drainage (PTBD). Most of these episodes are self-limited, however, in less than 5% of cases, hemobilia is clinically significant, and may require urgent intervention. Prompt diagnosis of major hemobilia causing hemodynamic instability can be challenging. We present a case of massive hemobilia due to hepatic arteriobiliary fistula formation after PTBD placement.
Case Description/Methods: A 47-year-old male with a large multiloculated liver abscess who had undergone placement of 2 indwelling hepatic drains and a percutaneous transhepatic biliary drain (PTBD) presented with increasing malodorous drain output. The PTBD was placed a month prior to relieve biliary obstruction from the abscess. During his clinical course, he began to have profuse frank sanguineous output from the PTBD with a rapid drop in hemoglobin along with hemodynamic instability. He was emergently taken to Interventional Radiology due to concern for a portal venous or hepatic arterial bleed. A digital subtraction angiogram (DSA) of the right hepatic artery demonstrated no active hemorrhage or pseudoaneurysm. Contrast injection of the PTBD showed filling defects consistent with hemorrhagic products and biliary dilation. The PTBD was retracted over a wire. Upon rapidly repeating a DSA, frank extravasation of contrast was seen from the right hepatic artery into the biliary tree. Upon localizing the source of the bleed, coil embolization of the branch of the right hepatic artery which had fistulized to the biliary tree was carried out. Post-embolization angiogram demonstrated successful closure of the fistula with no flow into the biliary tree. The PTBD was then exchanged for a new drain. The patient’s hemodynamic status stabilized after the procedure with no further drop in hemoglobin.
Discussion: Hemobilia can present with life-threatening bleeding as described above. In a series of 333 patients who underwent PTBD placement, hepatic arteriography was able to demonstrate the source of hemorrhage in all 13 patients who developed severe hemobilia. Four out of 13 patients had hepatic artery-bile duct fistulas. Thus, if significant hemobilia develops following PTBD, hepatic angiography should be performed at the earliest, not only to demonstrate the cause of the hemorrhage but also to attempt to control it.

Figure: Figure 1: (A) and (B) Digital Subtraction Angiogram demonstrating frank extravasation of contrast from the right hepatic artery into the biliary tree (arrows) (C) Angiogram post-coil embolization (arrow) demonstrating successful closure of the fistula with absence of flow into the biliary tree.
Disclosures:
Aishwarya Thakurdesai indicated no relevant financial relationships.
Bryan Glaenzer indicated no relevant financial relationships.
Ashwani Singal indicated no relevant financial relationships.
Dipendra Parajuli indicated no relevant financial relationships.
Aishwarya Thakurdesai, MBBS, Bryan Glaenzer, MD, Ashwani Singal, MD, MS, Dipendra Parajuli, MD. P3582 - Hepatic Arteriobiliary Fistula Causing Massive Hemobilia: Successful Treatment With Coil Embolization, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
