Tuesday Poster Session
Category: Biliary/Pancreas
P3588 - Penicillin or Cannabis? A Unique Case of Drug-Induced Necrotizing Pancreatitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ariana R. Tagliaferri, MD
Creighton University Medical Center
Phoenix, AZ
Presenting Author(s)
Ariana R. Tagliaferri, MD1, Danielle Tran, BS2, Indu Srinivasan, MD1
1Creighton University Medical Center, Phoenix, AZ; 2Creighton University School of Medicine, Omaha, NE
Introduction: Pancreatitis is often due to gallstones or alcohol, but other causes include hypertriglyceridemia, hypercalcemia, scorpion stings, autoimmune, malignancy or trauma. Drug-induced pancreatitis accounts for 0.1-2% of all cases. It’s a diagnosis of exclusion and likely under-recognized. Over 120 medications have been reported, although studies outlining these effects are limited. The commonest offenders are valproic acid, antihyperglycemics, statins, ACE inhibitors, diuretics, contraceptives and NSAID’s. There are only 5 cases of penicillin-induced pancreatitis. Cannabis accounts for 2-13% of drug-induced pancreatitis and is seen particularly in males under the age of 35. We present a case of drug-induced pancreatitis caused by recent use of amoxicillin-clavulanate and heavy tetrahydrocannabinol (THC) vaping.
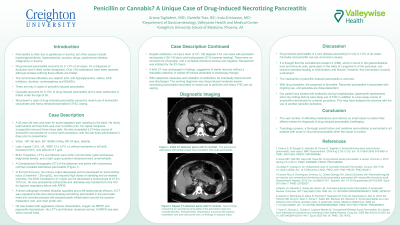
Case Description/Methods: A 32-year-old man presented with epigastric pain and was diagnosed with acute pancreatitis. He was tachycardic (150 bpm), hypertensive (164/90 mmHg) and tachypneic (34 bpm). Lipase was 7,315. An autoimmune panel, CMP, triglycerides, RUQ US and MRCP were unremarkable. He denied recent alcohol use, but vaped marijuana 3x daily. He completed a 2-week course of amoxicillin-clavulanate for a dental surgery with last dose taken 3 days before presentation. He was ultimately transferred to the ICU for septic shock and hypoxic respiratory failure with ARDS requiring BiPAP. A repeat CT revealed bibasilar opacities, left sided pleural effusion and necrotizing pancreatitis in the pancreatic head and uncinate process with peripancreatic inflammation around the SMV and main portal vein. Despite aggressive volume resuscitation and piperacillin-tazobactam, he was febrile (101℉) for one week with persistent tachycardia and leukocytosis (27.8 x 10^3/uL). A septic workup was negative. A third CT was suggestive of sterile necrosis without a drainable collection or walled-off lesions amenable to endoscopy. With supportive measures and cessation of antibiotics, he eventually improved. The diagnosis was drug-induced necrotizing pancreatitis secondary to recent penicillin use and THC vaping.
Discussion: Drug-induced pancreatitis is a rare disease, uncommonly caused by cannabis or penicillin. The vast number of offending medications and reliance on small cases to outline their effects makes the diagnosis challenging. Toxicology screens, a thorough social history and medicine reconciliation is warranted in all patients with acute or recurrent pancreatitis when the cause is unclear.
Disclosures:
Ariana R. Tagliaferri, MD1, Danielle Tran, BS2, Indu Srinivasan, MD1. P3588 - Penicillin or Cannabis? A Unique Case of Drug-Induced Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Creighton University Medical Center, Phoenix, AZ; 2Creighton University School of Medicine, Omaha, NE
Introduction: Pancreatitis is often due to gallstones or alcohol, but other causes include hypertriglyceridemia, hypercalcemia, scorpion stings, autoimmune, malignancy or trauma. Drug-induced pancreatitis accounts for 0.1-2% of all cases. It’s a diagnosis of exclusion and likely under-recognized. Over 120 medications have been reported, although studies outlining these effects are limited. The commonest offenders are valproic acid, antihyperglycemics, statins, ACE inhibitors, diuretics, contraceptives and NSAID’s. There are only 5 cases of penicillin-induced pancreatitis. Cannabis accounts for 2-13% of drug-induced pancreatitis and is seen particularly in males under the age of 35. We present a case of drug-induced pancreatitis caused by recent use of amoxicillin-clavulanate and heavy tetrahydrocannabinol (THC) vaping.
Case Description/Methods: A 32-year-old man presented with epigastric pain and was diagnosed with acute pancreatitis. He was tachycardic (150 bpm), hypertensive (164/90 mmHg) and tachypneic (34 bpm). Lipase was 7,315. An autoimmune panel, CMP, triglycerides, RUQ US and MRCP were unremarkable. He denied recent alcohol use, but vaped marijuana 3x daily. He completed a 2-week course of amoxicillin-clavulanate for a dental surgery with last dose taken 3 days before presentation. He was ultimately transferred to the ICU for septic shock and hypoxic respiratory failure with ARDS requiring BiPAP. A repeat CT revealed bibasilar opacities, left sided pleural effusion and necrotizing pancreatitis in the pancreatic head and uncinate process with peripancreatic inflammation around the SMV and main portal vein. Despite aggressive volume resuscitation and piperacillin-tazobactam, he was febrile (101℉) for one week with persistent tachycardia and leukocytosis (27.8 x 10^3/uL). A septic workup was negative. A third CT was suggestive of sterile necrosis without a drainable collection or walled-off lesions amenable to endoscopy. With supportive measures and cessation of antibiotics, he eventually improved. The diagnosis was drug-induced necrotizing pancreatitis secondary to recent penicillin use and THC vaping.
Discussion: Drug-induced pancreatitis is a rare disease, uncommonly caused by cannabis or penicillin. The vast number of offending medications and reliance on small cases to outline their effects makes the diagnosis challenging. Toxicology screens, a thorough social history and medicine reconciliation is warranted in all patients with acute or recurrent pancreatitis when the cause is unclear.
Disclosures:
Ariana Tagliaferri indicated no relevant financial relationships.
Danielle Tran indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Ariana R. Tagliaferri, MD1, Danielle Tran, BS2, Indu Srinivasan, MD1. P3588 - Penicillin or Cannabis? A Unique Case of Drug-Induced Necrotizing Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
