Tuesday Poster Session
Category: Biliary/Pancreas
P3595 - Unveiling the Enigma: A Case Report of Sphincter of Oddi Dysfunction Masquerading as Cannabis Hyperemesis Syndrome
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Guneet Sidhu, MD
University of North Dakota
Fargo, ND
Presenting Author(s)
Guneet Sidhu, MD1, Hussam Almasri, MD2, John Bassett, MD, FACG2, Laura Nichols, MD2
1University of North Dakota, Fargo, ND; 2Sanford Health, Fargo, ND
Introduction: Sphincter of Oddi dysfunction (SOD) is a complex hepatobiliary disorder often overlooked in clinical practice but significantly affecting patients' quality of life. This condition, primarily occurring post-cholecystectomy, presents with recurrent biliary colic symptoms, elevated aminotransferases, and pancreatitis.
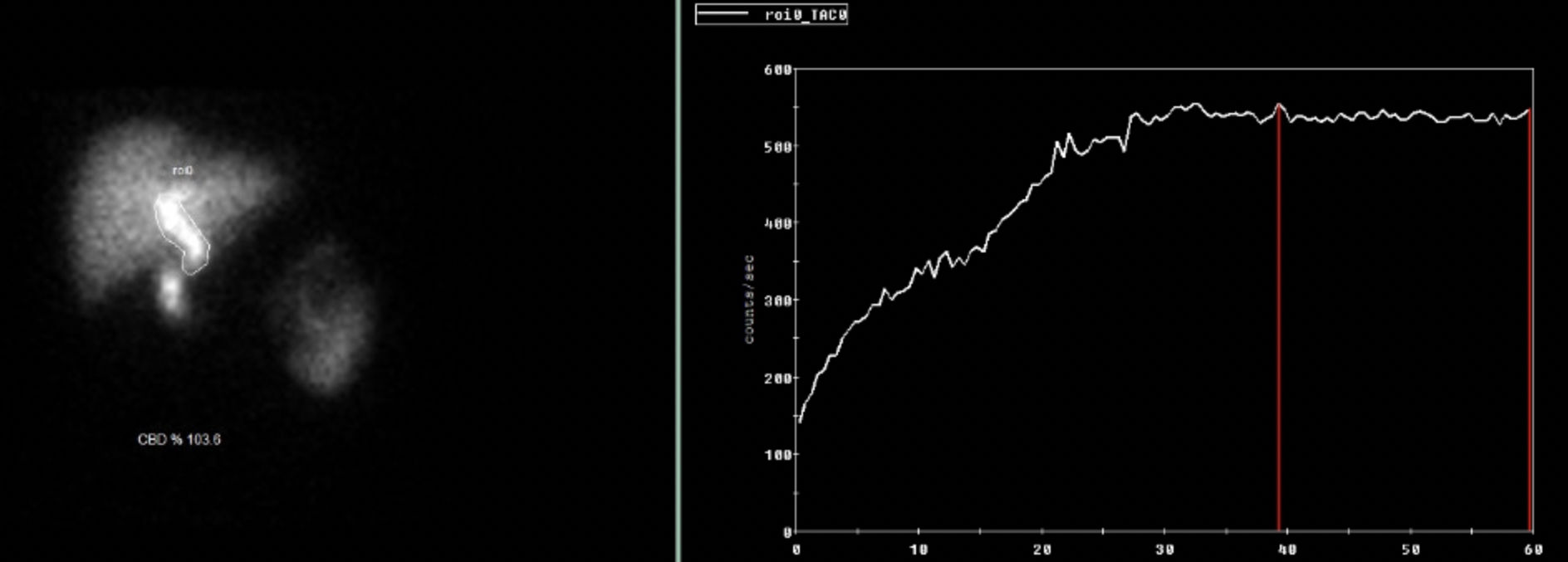
Case Description/Methods: A 30-year-old male presented to the ED with complaints of abdominal pain, nausea, vomiting, and diaphoresis that started while eating a meal. He had a history of cholecystectomy and cannabis use disorder. Labs revealed a normal CBC, elevated alkaline phosphatase (176 (U/L)), ALT (339 (U/L)), and AST (190 (U/L)). CRP and procal were normal. CT abdomen and pelvis was negative for any acute intra-abdominal process. Due to intractable nausea and abdominal pain, gastroenterology was consulted, as the patient experienced persistent intractable nausea, vomiting, and severe lower abdominal pain throughout the hospital stay. Notably, relief was only achieved with a hot shower, raising suspicion for cannabinoid hyperemesis syndrome despite the patient's denial of recent marijuana use. Viral hepatitis, autoimmune hepatitis, PT/INR and ceruloplasmin testing was normal. EGD showed normal esophagus and mildly erythematous mucosa in the gastric fundus. EUS demonstrated normal pancreatic morphology and mild dilation of the common bile duct with sharp tapering into the ampulla suggesting papillary stenosis. NM sphincter of Oddi scan was diagnostic for SOD, prompting ERCP, during which an 8 mm biliary sphincterotomy and temporary stent placement in the CBD were performed. Subsequently, the patient experienced remarkable resolution of nausea, vomiting, and abdominal pain, leading to discharge in stable condition.
Discussion: Our case demonstrates that in patients with intractable nausea, vomiting, abdominal pain and a history of cannabis use disorder, appropriate evaluation is needed to ensure an accurate diagnosis. SOD presents as a clinical syndrome, causing abdominal pain, enzyme elevations, and ductal abnormalities due to mechanical or functional anomalies in the biliary or pancreatic sphincter. Differential diagnosis, especially with diseases like cannabis hyperemesis syndrome, necessitates careful consideration given overlapping symptomatology and potential mismanagement implications. Treatment modalities vary based on SOD type, with endoscopic sphincterotomy (ERCP) being the preferred approach for biliary SOD, whereas total SO division is effective for pancreatic SOD.
Disclosures:
Guneet Sidhu, MD1, Hussam Almasri, MD2, John Bassett, MD, FACG2, Laura Nichols, MD2. P3595 - Unveiling the Enigma: A Case Report of Sphincter of Oddi Dysfunction Masquerading as Cannabis Hyperemesis Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Dakota, Fargo, ND; 2Sanford Health, Fargo, ND
Introduction: Sphincter of Oddi dysfunction (SOD) is a complex hepatobiliary disorder often overlooked in clinical practice but significantly affecting patients' quality of life. This condition, primarily occurring post-cholecystectomy, presents with recurrent biliary colic symptoms, elevated aminotransferases, and pancreatitis.
Case Description/Methods: A 30-year-old male presented to the ED with complaints of abdominal pain, nausea, vomiting, and diaphoresis that started while eating a meal. He had a history of cholecystectomy and cannabis use disorder. Labs revealed a normal CBC, elevated alkaline phosphatase (176 (U/L)), ALT (339 (U/L)), and AST (190 (U/L)). CRP and procal were normal. CT abdomen and pelvis was negative for any acute intra-abdominal process. Due to intractable nausea and abdominal pain, gastroenterology was consulted, as the patient experienced persistent intractable nausea, vomiting, and severe lower abdominal pain throughout the hospital stay. Notably, relief was only achieved with a hot shower, raising suspicion for cannabinoid hyperemesis syndrome despite the patient's denial of recent marijuana use. Viral hepatitis, autoimmune hepatitis, PT/INR and ceruloplasmin testing was normal. EGD showed normal esophagus and mildly erythematous mucosa in the gastric fundus. EUS demonstrated normal pancreatic morphology and mild dilation of the common bile duct with sharp tapering into the ampulla suggesting papillary stenosis. NM sphincter of Oddi scan was diagnostic for SOD, prompting ERCP, during which an 8 mm biliary sphincterotomy and temporary stent placement in the CBD were performed. Subsequently, the patient experienced remarkable resolution of nausea, vomiting, and abdominal pain, leading to discharge in stable condition.
Discussion: Our case demonstrates that in patients with intractable nausea, vomiting, abdominal pain and a history of cannabis use disorder, appropriate evaluation is needed to ensure an accurate diagnosis. SOD presents as a clinical syndrome, causing abdominal pain, enzyme elevations, and ductal abnormalities due to mechanical or functional anomalies in the biliary or pancreatic sphincter. Differential diagnosis, especially with diseases like cannabis hyperemesis syndrome, necessitates careful consideration given overlapping symptomatology and potential mismanagement implications. Treatment modalities vary based on SOD type, with endoscopic sphincterotomy (ERCP) being the preferred approach for biliary SOD, whereas total SO division is effective for pancreatic SOD.
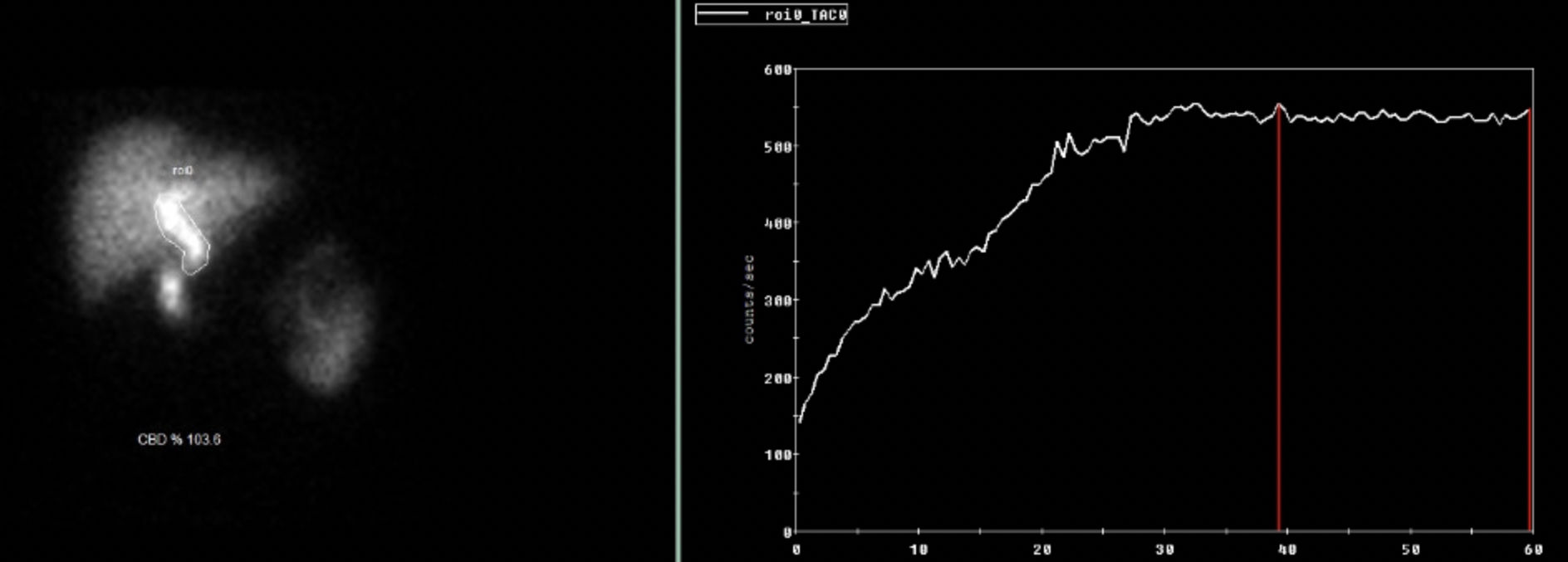
Figure: There is radiotracer stasis within the common duct, which is relatively persistent over the study.
Disclosures:
Guneet Sidhu indicated no relevant financial relationships.
Hussam Almasri indicated no relevant financial relationships.
John Bassett indicated no relevant financial relationships.
Laura Nichols indicated no relevant financial relationships.
Guneet Sidhu, MD1, Hussam Almasri, MD2, John Bassett, MD, FACG2, Laura Nichols, MD2. P3595 - Unveiling the Enigma: A Case Report of Sphincter of Oddi Dysfunction Masquerading as Cannabis Hyperemesis Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
