Tuesday Poster Session
Category: Biliary/Pancreas
P3596 - Emergence of Postoperative Pancreatitis: Unveiling the Rare Consequence of Non-Abdominal Surgery
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Guneet Sidhu, MD
University of North Dakota
Fargo, ND
Presenting Author(s)
Guneet Sidhu, MD1, Anil Sriramoju, MD2, John Bassett, MD, FACG3, Hasrat Khan, MD4
1University of North Dakota, Fargo, ND; 2University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 3Sanford Health, Fargo, ND; 4Sanford Medical Center, Fargo, ND
Introduction: Pancreatitis, particularly acute necrotizing pancreatitis, is a severe inflammatory condition of the pancreas that can arise as a postoperative complication. While commonly associated with abdominal surgeries such as cholecystectomy or pancreatic surgery, pancreatitis following non-abdominal procedures is rare and not well-documented in the literature.
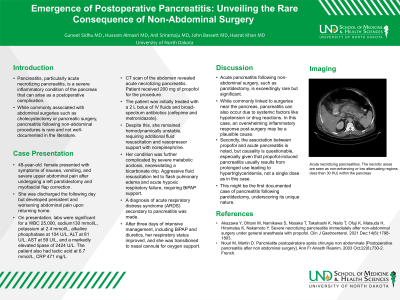
Case Description/Methods: 48Y female presented with symptoms of nausea, vomiting, and severe upper abdominal pain after undergoing a left parotidectomy and myofascial flap correction. She was discharged the following day but developed persistent and worsening abdominal pain upon returning home. On presentation, labs were significant for a WBC 25,000, sodium130 mmol/L, potassium at 2.4 mmol/L, alkaline phosphatase at 104 U/L, ALT at 81 U/L, AST at 59 U/L, and a markedly elevated lipase of 2424 U/L. The patient also had lactic acid at 6.7 mmol/L, CRP 471 mg/L. CT scan of the abdomen revealed acute necrotizing pancreatitis. Patient received 200 mg of propofol for the procedure. The patient was initially treated with a 2 L bolus of IV fluids and broad-spectrum antibiotics (cefepime and metronidazole). Despite this, she remained hemodynamically unstable, requiring additional fluid resuscitation and vasopressor support with norepinephrine. Her condition was further complicated by severe metabolic acidosis, necessitating a bicarbonate drip. Aggressive fluid resuscitation led to flash pulmonary edema and acute hypoxic respiratory failure, requiring BiPAP support. A diagnosis of acute respiratory distress syndrome (ARDS) secondary to pancreatitis was made. After three days of intensive management, including BiPAP and diuretics, her respiratory status improved, and she was transitioned to nasal cannula for oxygen support.
Discussion: Acute pancreatitis following non-abdominal surgery, such as parotidectomy, is exceedingly rare but significant. While commonly linked to surgeries near the pancreas, pancreatitis can also occur due to systemic factors like hypotension or drug reactions. In this case, an overwhelming inflammatory response post-surgery may be a plausible cause. Second, the association between propofol and acute pancreatitis is noted, but causality is questionable, especially given that propofol-induced pancreatitis usually results from prolonged use leading to hypertriglyceridemia, not a single dose as in this case. This might be the first documented case of pancreatitis following parotidectomy, underscoring its unique nature.
Disclosures:
Guneet Sidhu, MD1, Anil Sriramoju, MD2, John Bassett, MD, FACG3, Hasrat Khan, MD4. P3596 - Emergence of Postoperative Pancreatitis: Unveiling the Rare Consequence of Non-Abdominal Surgery, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Dakota, Fargo, ND; 2University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 3Sanford Health, Fargo, ND; 4Sanford Medical Center, Fargo, ND
Introduction: Pancreatitis, particularly acute necrotizing pancreatitis, is a severe inflammatory condition of the pancreas that can arise as a postoperative complication. While commonly associated with abdominal surgeries such as cholecystectomy or pancreatic surgery, pancreatitis following non-abdominal procedures is rare and not well-documented in the literature.
Case Description/Methods: 48Y female presented with symptoms of nausea, vomiting, and severe upper abdominal pain after undergoing a left parotidectomy and myofascial flap correction. She was discharged the following day but developed persistent and worsening abdominal pain upon returning home. On presentation, labs were significant for a WBC 25,000, sodium130 mmol/L, potassium at 2.4 mmol/L, alkaline phosphatase at 104 U/L, ALT at 81 U/L, AST at 59 U/L, and a markedly elevated lipase of 2424 U/L. The patient also had lactic acid at 6.7 mmol/L, CRP 471 mg/L. CT scan of the abdomen revealed acute necrotizing pancreatitis. Patient received 200 mg of propofol for the procedure. The patient was initially treated with a 2 L bolus of IV fluids and broad-spectrum antibiotics (cefepime and metronidazole). Despite this, she remained hemodynamically unstable, requiring additional fluid resuscitation and vasopressor support with norepinephrine. Her condition was further complicated by severe metabolic acidosis, necessitating a bicarbonate drip. Aggressive fluid resuscitation led to flash pulmonary edema and acute hypoxic respiratory failure, requiring BiPAP support. A diagnosis of acute respiratory distress syndrome (ARDS) secondary to pancreatitis was made. After three days of intensive management, including BiPAP and diuretics, her respiratory status improved, and she was transitioned to nasal cannula for oxygen support.
Discussion: Acute pancreatitis following non-abdominal surgery, such as parotidectomy, is exceedingly rare but significant. While commonly linked to surgeries near the pancreas, pancreatitis can also occur due to systemic factors like hypotension or drug reactions. In this case, an overwhelming inflammatory response post-surgery may be a plausible cause. Second, the association between propofol and acute pancreatitis is noted, but causality is questionable, especially given that propofol-induced pancreatitis usually results from prolonged use leading to hypertriglyceridemia, not a single dose as in this case. This might be the first documented case of pancreatitis following parotidectomy, underscoring its unique nature.
Disclosures:
Guneet Sidhu indicated no relevant financial relationships.
Anil Sriramoju indicated no relevant financial relationships.
John Bassett indicated no relevant financial relationships.
Hasrat Khan indicated no relevant financial relationships.
Guneet Sidhu, MD1, Anil Sriramoju, MD2, John Bassett, MD, FACG3, Hasrat Khan, MD4. P3596 - Emergence of Postoperative Pancreatitis: Unveiling the Rare Consequence of Non-Abdominal Surgery, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
