Tuesday Poster Session
Category: Biliary/Pancreas
P3599 - Disappearing Bile Duct Adenoma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Uday Patel, DO
Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Uday Patel, DO1, Sunay Patel, DO1, Bryant Javier, DO1, Simran Kumari, MBBS2, Piryanka Kumari, MD1, Sung K. Yang, MD1
1Parkview Medical Center, Pueblo, CO; 2Peoples University of Medical and Health Sciences for Women, Karachi, Sindh, Pakistan
Introduction: Bile duct adenomas (BDA) are rare, benign tumors of the biliary tract which are thought to make up <2% of primary hepatobiliary lesions, however given the fact that these lesions are mostly diagnosed incidentally or at time of autopsy, true incidence is difficult to ascertain. BDA occur at similar rates between genders and can present with symptoms of cholestasis. BDA are treated by curative resection due to risks of recurrence and transformation to cholangiocarcinoma. Here, we describe a case in which a BDA was confirmed by histopathology but disappeared spontaneously.
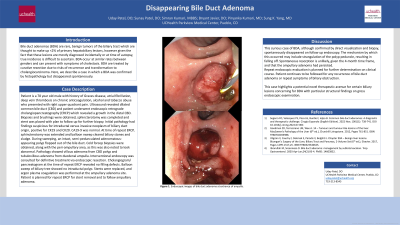
Case Description/Methods: 78 year old male with history of Graves disease, atrial fibrillation, deep vein thrombosis on chronic anticoagulation, alcohol and tobacco abuse presented with right upper quadrant pain. Ultrasound revealed dilated common bile duct (CBD) and patient underwent endoscopic retrograde cholangiopancreatography (ERCP) which revealed a growth in the distal CBD. Biopsies and brushings were obtained, sphincterotomy was completed and stent was placed with plan to follow up for further biopsy. Initial pathology had findings suspicious for intraductal versus invasive neoplasm of biliary duct origin, positive for CK19 and CK20. CA19-9 was normal. At time of repeat ERCP, sphincterotomy was extended and balloon sweep cleared biliary stones and sludge. During sweeping, an intact, semi-pedunculated adenomatous-appearing polyp flopped out of the bile duct. Cold forep biopsies were obtained, along with the peri-ampullary area, as this was also noted to look abnormal. Pathology showed villous adenoma from CBD polyp and tubulovillous adenoma from duodenal ampulla. Interventional endoscopy was consulted for definitive treatment via endoscopic resection. Cholangiogram/ pancreatogram at the time of repeat ERCP revealed no filling defects. Balloon sweep of biliary tree showed no intraductal polyp. Stents were replaced, and argon plasma coagulation was performed at the ampullary adenoma site. Patient is planned for repeat ERCP for stent removal and to follow ampullary adenoma.
Discussion: This curious case of BDA, although confirmed by direct visualization and biopsy, spontaneously disappeared on follow up endoscopy. The mechanism by which this occurred may include strangulation of the polyp peduncle, resulting in falling off. Spontaneous resorption is unlikely, given the 4-month time frame, and that the ampullary adenoma had persisted. Repeat endoscopic evaluation is planned for further determination on clinical course.

Disclosures:
Uday Patel, DO1, Sunay Patel, DO1, Bryant Javier, DO1, Simran Kumari, MBBS2, Piryanka Kumari, MD1, Sung K. Yang, MD1. P3599 - Disappearing Bile Duct Adenoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Parkview Medical Center, Pueblo, CO; 2Peoples University of Medical and Health Sciences for Women, Karachi, Sindh, Pakistan
Introduction: Bile duct adenomas (BDA) are rare, benign tumors of the biliary tract which are thought to make up <2% of primary hepatobiliary lesions, however given the fact that these lesions are mostly diagnosed incidentally or at time of autopsy, true incidence is difficult to ascertain. BDA occur at similar rates between genders and can present with symptoms of cholestasis. BDA are treated by curative resection due to risks of recurrence and transformation to cholangiocarcinoma. Here, we describe a case in which a BDA was confirmed by histopathology but disappeared spontaneously.
Case Description/Methods: 78 year old male with history of Graves disease, atrial fibrillation, deep vein thrombosis on chronic anticoagulation, alcohol and tobacco abuse presented with right upper quadrant pain. Ultrasound revealed dilated common bile duct (CBD) and patient underwent endoscopic retrograde cholangiopancreatography (ERCP) which revealed a growth in the distal CBD. Biopsies and brushings were obtained, sphincterotomy was completed and stent was placed with plan to follow up for further biopsy. Initial pathology had findings suspicious for intraductal versus invasive neoplasm of biliary duct origin, positive for CK19 and CK20. CA19-9 was normal. At time of repeat ERCP, sphincterotomy was extended and balloon sweep cleared biliary stones and sludge. During sweeping, an intact, semi-pedunculated adenomatous-appearing polyp flopped out of the bile duct. Cold forep biopsies were obtained, along with the peri-ampullary area, as this was also noted to look abnormal. Pathology showed villous adenoma from CBD polyp and tubulovillous adenoma from duodenal ampulla. Interventional endoscopy was consulted for definitive treatment via endoscopic resection. Cholangiogram/ pancreatogram at the time of repeat ERCP revealed no filling defects. Balloon sweep of biliary tree showed no intraductal polyp. Stents were replaced, and argon plasma coagulation was performed at the ampullary adenoma site. Patient is planned for repeat ERCP for stent removal and to follow ampullary adenoma.
Discussion: This curious case of BDA, although confirmed by direct visualization and biopsy, spontaneously disappeared on follow up endoscopy. The mechanism by which this occurred may include strangulation of the polyp peduncle, resulting in falling off. Spontaneous resorption is unlikely, given the 4-month time frame, and that the ampullary adenoma had persisted. Repeat endoscopic evaluation is planned for further determination on clinical course.

Figure: Bile Duct Adenoma
Disclosures:
Uday Patel indicated no relevant financial relationships.
Sunay Patel indicated no relevant financial relationships.
Bryant Javier indicated no relevant financial relationships.
Simran Kumari indicated no relevant financial relationships.
Piryanka Kumari indicated no relevant financial relationships.
Sung Yang indicated no relevant financial relationships.
Uday Patel, DO1, Sunay Patel, DO1, Bryant Javier, DO1, Simran Kumari, MBBS2, Piryanka Kumari, MD1, Sung K. Yang, MD1. P3599 - Disappearing Bile Duct Adenoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
