Tuesday Poster Session
Category: Biliary/Pancreas
P3425 - Risk of Venous Thromboembolism in Acute Necrotizing Pancreatitis: A Propensity-Matched Analysis From a Multicenter US Cohort Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Azizullah Beran, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Azizullah Beran, MD1, Osama Hamid, MD2, Mouhand F.H. Mohamed, MD, MSc3, John Guardiola, MD1, Indira Bhavsar-Burke, MD, MHPE2, Thomas Maatman, MD4, Nicholas Zyromski, MD5, Itegbemie Obaitan, MD, MPH1, Nasir Saleem, MD1, Mohammad Al-Haddad, MD, FACG1, Evan L. Fogel, MSc, MD6, Jeffrey Easler, MD1, Mark A. Gromski, MD1
1Indiana University School of Medicine, Indianapolis, IN; 2University of Texas Southwestern Medical Center, Dallas, TX; 3Mayo Clinic, Rochester, MN; 4Indiana University, Indianapolis, IN; 5Indianapolis, IN; 6IFMC9W, Indianapolis, IN
Introduction: Acute pancreatitis (AP) is a leading cause of gastrointestinal-related hospital admissions in the U.S. Up to 20% of AP cases can progress to acute necrotizing pancreatitis (ANP), a severe systemic inflammatory condition. ANP is often associated with prolonged hospitalization, immobility, and central venous access, all of which can contribute to a hypercoagulable state and an increased risk of venous thromboembolism (VTE). Data on the risk of VTE in patients with ANP is limited. We aimed to assess the risk of VTE in patients with ANP compared to acute interstitial edematous pancreatitis (AEP) without necrosis.
Methods: This is a retrospective United States-based, propensity-matched cohort study. We analyzed the U.S. Collaborative Network in the TriNetX platform to include adult patients diagnosed with AP from 2014 to 2024. We excluded patients with prior portal vein thrombosis (PVT) or VTE. We compared the risk of VTE and PVT within 30 days of AP diagnosis between the ANP and AEP cohorts, using one-to-one propensity score matching for known VTE risk factors. After propensity matching, we calculated the outcomes and expressed them as odds ratios (ORs) with 95% confidence intervals (CI). A two-sided p-value of < 0.05 was considered statistically significant. The primary outcome was the risk of VTE, a composite of extremity deep venous thrombosis (eDVT) and pulmonary embolism (PE). Secondary outcomes were the risk of eDVT, PE, and PVT.
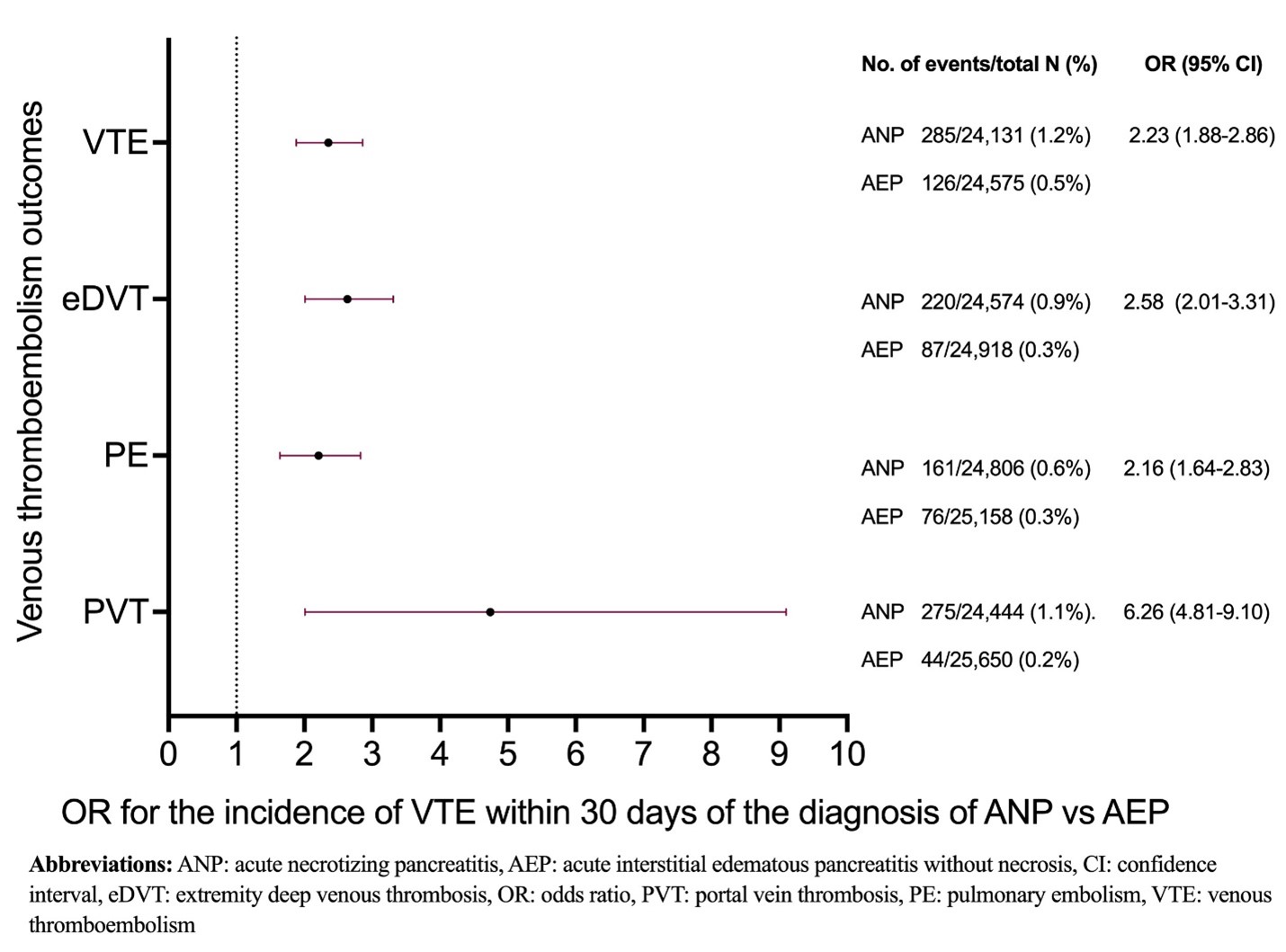
Results: After one-to-one propensity score matching was performed for several confounders between the cohorts (Table 1), there were a total of 51,950 patients with AP in the final analysis (25,975 in the ANP cohort and 25,975 in the matched AEP cohort). The risk of VTE (1.2% vs. 0.5%, OR 2.23, 95% CI 1.88-2.86, p< 0.001, Figure 1), eDVT (0.9% vs. 0.3%, OR 2.58, 95% CI 2.01-3.31, p< 0.001), PE (0.6% vs. 0.3%, OR 2.16, 95% CI 1.64-2.83, p< 0.001), and PVT (1.1% vs. 0.2%, OR 6.62, 95% CI 4.81-9.1, p< 0.001) was significantly higher in patients with ANP compared to patients with AEP (Figure 1).
Discussion: Patients with ANP are at an increased risk of VTE compared to AEP patients. This finding underscores the necessity for physicians to maintain a high level of suspicion for VTE in this high-risk population. Further research is needed to investigate the impact of routine weekly ultrasound screening on the clinical outcomes of this select cohort of patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Azizullah Beran, MD1, Osama Hamid, MD2, Mouhand F.H. Mohamed, MD, MSc3, John Guardiola, MD1, Indira Bhavsar-Burke, MD, MHPE2, Thomas Maatman, MD4, Nicholas Zyromski, MD5, Itegbemie Obaitan, MD, MPH1, Nasir Saleem, MD1, Mohammad Al-Haddad, MD, FACG1, Evan L. Fogel, MSc, MD6, Jeffrey Easler, MD1, Mark A. Gromski, MD1. P3425 - Risk of Venous Thromboembolism in Acute Necrotizing Pancreatitis: A Propensity-Matched Analysis From a Multicenter US Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2University of Texas Southwestern Medical Center, Dallas, TX; 3Mayo Clinic, Rochester, MN; 4Indiana University, Indianapolis, IN; 5Indianapolis, IN; 6IFMC9W, Indianapolis, IN
Introduction: Acute pancreatitis (AP) is a leading cause of gastrointestinal-related hospital admissions in the U.S. Up to 20% of AP cases can progress to acute necrotizing pancreatitis (ANP), a severe systemic inflammatory condition. ANP is often associated with prolonged hospitalization, immobility, and central venous access, all of which can contribute to a hypercoagulable state and an increased risk of venous thromboembolism (VTE). Data on the risk of VTE in patients with ANP is limited. We aimed to assess the risk of VTE in patients with ANP compared to acute interstitial edematous pancreatitis (AEP) without necrosis.
Methods: This is a retrospective United States-based, propensity-matched cohort study. We analyzed the U.S. Collaborative Network in the TriNetX platform to include adult patients diagnosed with AP from 2014 to 2024. We excluded patients with prior portal vein thrombosis (PVT) or VTE. We compared the risk of VTE and PVT within 30 days of AP diagnosis between the ANP and AEP cohorts, using one-to-one propensity score matching for known VTE risk factors. After propensity matching, we calculated the outcomes and expressed them as odds ratios (ORs) with 95% confidence intervals (CI). A two-sided p-value of < 0.05 was considered statistically significant. The primary outcome was the risk of VTE, a composite of extremity deep venous thrombosis (eDVT) and pulmonary embolism (PE). Secondary outcomes were the risk of eDVT, PE, and PVT.
Results: After one-to-one propensity score matching was performed for several confounders between the cohorts (Table 1), there were a total of 51,950 patients with AP in the final analysis (25,975 in the ANP cohort and 25,975 in the matched AEP cohort). The risk of VTE (1.2% vs. 0.5%, OR 2.23, 95% CI 1.88-2.86, p< 0.001, Figure 1), eDVT (0.9% vs. 0.3%, OR 2.58, 95% CI 2.01-3.31, p< 0.001), PE (0.6% vs. 0.3%, OR 2.16, 95% CI 1.64-2.83, p< 0.001), and PVT (1.1% vs. 0.2%, OR 6.62, 95% CI 4.81-9.1, p< 0.001) was significantly higher in patients with ANP compared to patients with AEP (Figure 1).
Discussion: Patients with ANP are at an increased risk of VTE compared to AEP patients. This finding underscores the necessity for physicians to maintain a high level of suspicion for VTE in this high-risk population. Further research is needed to investigate the impact of routine weekly ultrasound screening on the clinical outcomes of this select cohort of patients.
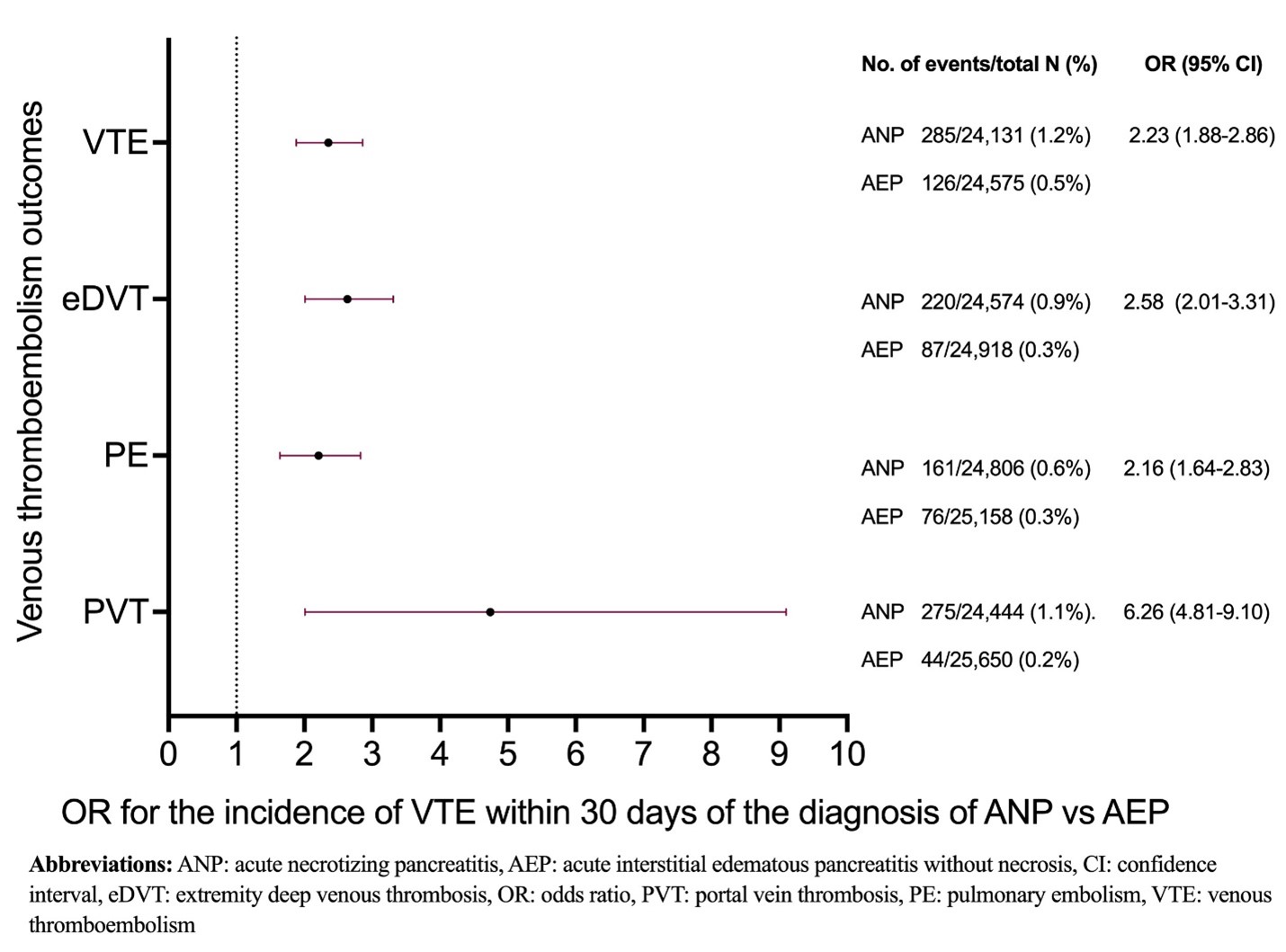
Figure: Figure 1: Venous thromboembolism outcomes between ANP and AEP cohorts after propensity-score matching.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Azizullah Beran indicated no relevant financial relationships.
Osama Hamid indicated no relevant financial relationships.
Mouhand Mohamed indicated no relevant financial relationships.
John Guardiola: Boston Scientific Corporation – Travel Support. Olympus Corporation – Travel Support.
Indira Bhavsar-Burke indicated no relevant financial relationships.
Thomas Maatman indicated no relevant financial relationships.
Nicholas Zyromski indicated no relevant financial relationships.
Itegbemie Obaitan indicated no relevant financial relationships.
Nasir Saleem indicated no relevant financial relationships.
Mohammad Al-Haddad: Amplified Sciences – Grant/Research Support. Boston Scientific – Consultant. Interpace Diagnostics – Consultant.
Evan Fogel indicated no relevant financial relationships.
Jeffrey Easler: Boston Scientific – Consultant.
Mark Gromski: Allurion – Grant/Research Support. Ambu – Consultant. Boston Scientific – Consultant. Cook Medical – Grant/Research Support. Fractyl – Grant/Research Support.
Azizullah Beran, MD1, Osama Hamid, MD2, Mouhand F.H. Mohamed, MD, MSc3, John Guardiola, MD1, Indira Bhavsar-Burke, MD, MHPE2, Thomas Maatman, MD4, Nicholas Zyromski, MD5, Itegbemie Obaitan, MD, MPH1, Nasir Saleem, MD1, Mohammad Al-Haddad, MD, FACG1, Evan L. Fogel, MSc, MD6, Jeffrey Easler, MD1, Mark A. Gromski, MD1. P3425 - Risk of Venous Thromboembolism in Acute Necrotizing Pancreatitis: A Propensity-Matched Analysis From a Multicenter US Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
