Tuesday Poster Session
Category: Biliary/Pancreas
P3427 - Trends, Comparison of Treatment Modalities in Pancreatic Pseudocyst, and Predictors of 30-Day Readmissions Using National Readmission Database
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SK
Shahryar Khan, MD
University of Kansas
Overland Park, KS
Presenting Author(s)
Shahryar Khan, MD1, Mashal Alam Khan, MBBS2, Qazi Muhammad Safwan, MBBS3, Muhammad Abu Bakkar, MBBS4, Ahmed Khan Jadoon, MD5, Zarlish Rehman, MBBS6
1University of Kansas, Overland Park, KS; 2Khyber Medical University, Overland Park, KS; 3Khyber Medical College, Philadelphia, PA; 4Khyber Teaching Hospital, Peshawar, North-West Frontier, Pakistan; 5The Aga Khan University Hospital, Karachi City, Sindh, Pakistan; 6Hayatabad Medical Complex, Peshawar, North-West Frontier, Pakistan
Introduction: Pancreatic Pseudocyst (PP) is a common and unfavorable sequelae of acute and chronic pancreatitis. Due to symptoms, wide variation in the pseudocyst size, and associated comorbidities have led to conclusions that not all pseudocysts need to be intervened. Various treatment options for pancreatic pseudocysts have been described with conflicting conclusions. Surgical Drainage (SD) has been associated with various complications, Percutaneous (PD) and Endoscopic drainage (ED) of these collections has gained acceptance as an alternative to surgical drainage.
Methods: We retrospectively analyzed Nationwide Readmissions Database from 2018 to 2020 to identify patients hospitalized with PP. Discharges were included if they were adults, urgent/emergent and had a principal ICD-10 CM code indicating PP, and different treatment modalities including ED, PD, and SD. We compared trends of treatment modalities, mortality during index hospitalization, readmission rates, and resource utilization including hospital length of stay (LOS), and total hospitalization charges (THC). Independent risk factors for readmission were identified using multivariate cox regression analysis.
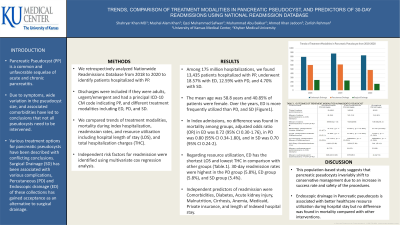
Results: Among 175 million hospitalizations, we found 13,435 patients hospitalized with PP, underwent 18.57% with ED, 12.59% with PD, and 4.70% with SD. The mean age was 58.8 years and 40.85% of patients were female. Over the years, ED is more frequently utilized than PD, and SD (Figure1). In Index admissions, no difference was found in mortality among groups, adjusted odds ratio (OR) in ED was 0.72 (95% CI 0.30-1.76), in PD was 0.80 (95% CI 0.34-1.80), and in SD was 0.70 (95% CI 0.24-2). Regarding resource utilization, ED has the shortest LOS and lowest THC in comparison with other groups (Table.1). 30-day readmission rates were highest in the PD group (5.8%), ED group (5.8%), and SD group (5.4%). Independent predictors of readmission were Comorbidities, Diabetes, Acute kidney injury, Malnutrition, Cirrhosis, Anemia, Medicaid, Private insurance, and length of Indexed hospital stay.
Discussion: This population-based study suggests that pancreatic pseudocysts invariably shift to conservative management due to an increase in success rate and safety of the procedures. Endoscopic drainage in Pancreatic pseudocysts is associated with better healthcare resource utilization during hospital stay but no difference was found in mortality compared with other interventions.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shahryar Khan, MD1, Mashal Alam Khan, MBBS2, Qazi Muhammad Safwan, MBBS3, Muhammad Abu Bakkar, MBBS4, Ahmed Khan Jadoon, MD5, Zarlish Rehman, MBBS6. P3427 - Trends, Comparison of Treatment Modalities in Pancreatic Pseudocyst, and Predictors of 30-Day Readmissions Using National Readmission Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas, Overland Park, KS; 2Khyber Medical University, Overland Park, KS; 3Khyber Medical College, Philadelphia, PA; 4Khyber Teaching Hospital, Peshawar, North-West Frontier, Pakistan; 5The Aga Khan University Hospital, Karachi City, Sindh, Pakistan; 6Hayatabad Medical Complex, Peshawar, North-West Frontier, Pakistan
Introduction: Pancreatic Pseudocyst (PP) is a common and unfavorable sequelae of acute and chronic pancreatitis. Due to symptoms, wide variation in the pseudocyst size, and associated comorbidities have led to conclusions that not all pseudocysts need to be intervened. Various treatment options for pancreatic pseudocysts have been described with conflicting conclusions. Surgical Drainage (SD) has been associated with various complications, Percutaneous (PD) and Endoscopic drainage (ED) of these collections has gained acceptance as an alternative to surgical drainage.
Methods: We retrospectively analyzed Nationwide Readmissions Database from 2018 to 2020 to identify patients hospitalized with PP. Discharges were included if they were adults, urgent/emergent and had a principal ICD-10 CM code indicating PP, and different treatment modalities including ED, PD, and SD. We compared trends of treatment modalities, mortality during index hospitalization, readmission rates, and resource utilization including hospital length of stay (LOS), and total hospitalization charges (THC). Independent risk factors for readmission were identified using multivariate cox regression analysis.
Results: Among 175 million hospitalizations, we found 13,435 patients hospitalized with PP, underwent 18.57% with ED, 12.59% with PD, and 4.70% with SD. The mean age was 58.8 years and 40.85% of patients were female. Over the years, ED is more frequently utilized than PD, and SD (Figure1). In Index admissions, no difference was found in mortality among groups, adjusted odds ratio (OR) in ED was 0.72 (95% CI 0.30-1.76), in PD was 0.80 (95% CI 0.34-1.80), and in SD was 0.70 (95% CI 0.24-2). Regarding resource utilization, ED has the shortest LOS and lowest THC in comparison with other groups (Table.1). 30-day readmission rates were highest in the PD group (5.8%), ED group (5.8%), and SD group (5.4%). Independent predictors of readmission were Comorbidities, Diabetes, Acute kidney injury, Malnutrition, Cirrhosis, Anemia, Medicaid, Private insurance, and length of Indexed hospital stay.
Discussion: This population-based study suggests that pancreatic pseudocysts invariably shift to conservative management due to an increase in success rate and safety of the procedures. Endoscopic drainage in Pancreatic pseudocysts is associated with better healthcare resource utilization during hospital stay but no difference was found in mortality compared with other interventions.

Figure: Figure.1 Trends of Treatment Modalities in Pancreatic Pseudocyst from 2018 to 2020.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shahryar Khan indicated no relevant financial relationships.
Mashal Alam Khan indicated no relevant financial relationships.
Qazi Muhammad Safwan indicated no relevant financial relationships.
Muhammad Abu Bakkar indicated no relevant financial relationships.
Ahmed Khan Jadoon indicated no relevant financial relationships.
Zarlish Rehman indicated no relevant financial relationships.
Shahryar Khan, MD1, Mashal Alam Khan, MBBS2, Qazi Muhammad Safwan, MBBS3, Muhammad Abu Bakkar, MBBS4, Ahmed Khan Jadoon, MD5, Zarlish Rehman, MBBS6. P3427 - Trends, Comparison of Treatment Modalities in Pancreatic Pseudocyst, and Predictors of 30-Day Readmissions Using National Readmission Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
