Tuesday Poster Session
Category: Biliary/Pancreas
P3428 - Utilization of Neoadjuvant Therapy for Pancreatic Ductal Adenocarcinoma in an Academic Rural Health Care System: A Large Multi-Center Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- VK
Vyshnavi Kodali, DO
Geisinger Medical Center
Danville, PA
Presenting Author(s)
Vyshnavi Kodali, DO1, Konstantinos Damiris, DO1, Malak Al-Bitar, MD2, Idorenyin Udoeyo, MPH2, Bradley D.. Confer, DO2
1Geisinger Medical Center, Danville, PA; 2Geisinger Health System, Danville, PA
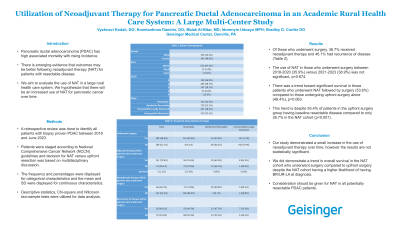
Introduction: Pancreatic ductal adenocarcinoma (PDAC) has high associated mortality with rising incidence. There is emerging evidence that outcomes may be better following neoadjuvant therapy (NAT) for patients with resectable disease. We aim to evaluate the use of NAT in a large rural health care system. We hypothesize that there will be an increased use of NAT for pancreatic cancer over time.
Methods: A retrospective review was done to identify all patients with biopsy proven PDAC between 2018 and June 2023. Patients were staged according to NCCN guidelines and decision for NAT versus upfront resection was based on multidisciplinary discussion. The frequency and percentages were displayed for categorical characteristics; the mean and SD for continuous characteristics. Descriptive statistics, Chi-square and Wilcoxon two-sample tests were utilized for data analysis.
Results: Out of 587 cases of confirmed PDAC, 180 patients were identified who underwent surgery. The median age at diagnosis was 70 years, with 50.4% males and 97.4% Caucasian. Most patients were classified as either ECOG 0 (26.9%) or ECOG 1 (48.7%) at time of diagnosis. The staging of disease was as follows: 22.3% resectable (R), 22.2% borderline resectable (BR), 18.2% unresectable locally advanced (UR-LA), 37.3% unresectable metastatic (UR-M). Of those who underwent surgery, 36.7% had neoadjuvant therapy and 46.1% had recurrence of disease (Table 1). The use of NAT in those who underwent surgery between 2018-2020 (35.9%) versus 2021-2023 (38.9%) was not significant, p=0.674. There was a trend toward significant survival in those patients who underwent NAT followed by surgery (53.6%) compared to those undergoing upfront surgery alone (49.4%), p=0.063. This trend is despite 93.4% of patients in the upfront surgery group having baseline resectable disease compared to only 26.7% in the NAT cohort, p< 0.001.
Discussion: Our study demonstrated a small increase in the use of neoadjuvant therapy over time, however the results are not statistically significant. We did demonstrate a trend in overall survival in the NAT cohort who underwent surgery compared to upfront surgery despite the NAT cohort having a higher likelihood of having BR/UR-LA at diagnosis. Consideration should be given for NAT in all potentially resectable PDAC patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Vyshnavi Kodali, DO1, Konstantinos Damiris, DO1, Malak Al-Bitar, MD2, Idorenyin Udoeyo, MPH2, Bradley D.. Confer, DO2. P3428 - Utilization of Neoadjuvant Therapy for Pancreatic Ductal Adenocarcinoma in an Academic Rural Health Care System: A Large Multi-Center Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Geisinger Medical Center, Danville, PA; 2Geisinger Health System, Danville, PA
Introduction: Pancreatic ductal adenocarcinoma (PDAC) has high associated mortality with rising incidence. There is emerging evidence that outcomes may be better following neoadjuvant therapy (NAT) for patients with resectable disease. We aim to evaluate the use of NAT in a large rural health care system. We hypothesize that there will be an increased use of NAT for pancreatic cancer over time.
Methods: A retrospective review was done to identify all patients with biopsy proven PDAC between 2018 and June 2023. Patients were staged according to NCCN guidelines and decision for NAT versus upfront resection was based on multidisciplinary discussion. The frequency and percentages were displayed for categorical characteristics; the mean and SD for continuous characteristics. Descriptive statistics, Chi-square and Wilcoxon two-sample tests were utilized for data analysis.
Results: Out of 587 cases of confirmed PDAC, 180 patients were identified who underwent surgery. The median age at diagnosis was 70 years, with 50.4% males and 97.4% Caucasian. Most patients were classified as either ECOG 0 (26.9%) or ECOG 1 (48.7%) at time of diagnosis. The staging of disease was as follows: 22.3% resectable (R), 22.2% borderline resectable (BR), 18.2% unresectable locally advanced (UR-LA), 37.3% unresectable metastatic (UR-M). Of those who underwent surgery, 36.7% had neoadjuvant therapy and 46.1% had recurrence of disease (Table 1). The use of NAT in those who underwent surgery between 2018-2020 (35.9%) versus 2021-2023 (38.9%) was not significant, p=0.674. There was a trend toward significant survival in those patients who underwent NAT followed by surgery (53.6%) compared to those undergoing upfront surgery alone (49.4%), p=0.063. This trend is despite 93.4% of patients in the upfront surgery group having baseline resectable disease compared to only 26.7% in the NAT cohort, p< 0.001.
Discussion: Our study demonstrated a small increase in the use of neoadjuvant therapy over time, however the results are not statistically significant. We did demonstrate a trend in overall survival in the NAT cohort who underwent surgery compared to upfront surgery despite the NAT cohort having a higher likelihood of having BR/UR-LA at diagnosis. Consideration should be given for NAT in all potentially resectable PDAC patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Vyshnavi Kodali indicated no relevant financial relationships.
Konstantinos Damiris indicated no relevant financial relationships.
Malak Al-Bitar indicated no relevant financial relationships.
Idorenyin Udoeyo indicated no relevant financial relationships.
Bradley Confer: Boston Scientific Corporation – Consultant. Exact Sciences – Advisory Committee/Board Member, FDA advisory panel.
Vyshnavi Kodali, DO1, Konstantinos Damiris, DO1, Malak Al-Bitar, MD2, Idorenyin Udoeyo, MPH2, Bradley D.. Confer, DO2. P3428 - Utilization of Neoadjuvant Therapy for Pancreatic Ductal Adenocarcinoma in an Academic Rural Health Care System: A Large Multi-Center Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
