Tuesday Poster Session
Category: Biliary/Pancreas
P3430 - Hospitalization Outcomes and Mortality Trends Among Patients With Thromboembolic Disease in Acute Pancreatitis: A Nationwide Inpatient Sample Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SB
Sheena Bhushan, MD
Northeast Georgia Medical Center
Buford, GA
Presenting Author(s)
Sheena Bhushan, MD1, Riaz Mahmood, MD1, Shane Robinson, MS2, Nikki Nikzad, MS3, Aja McCutchen, MD4
1Northeast Georgia Medical Center, Buford, GA; 2Northeast Georgia Medical Center, Gainesville, GA; 3Liver Institute Northwest, Seattle, WA; 4Atlanta Gastroenterology Associates, Atlanta, GA
Introduction: There is limited research evaluating outcomes of patients with acute pancreatitis and thromboembolic disease. This study aims to evaluate the influence of deep vein thrombosis (DVT) or pulmonary emboli (PE) on the outcomes of patients presenting with acute pancreatitis utilizing the National Inpatient Sample (NIS) database from 2016 to 2018.
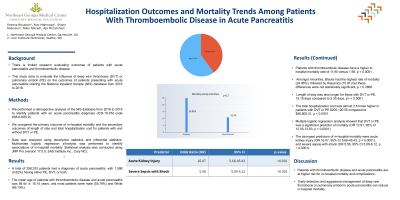
Methods: We performed a retrospective analysis of the NIS database from 2016 to 2018 to identify patients with an acute pancreatitis diagnosis (ICD-10-CM code K85.0-K85.9). We compared the primary outcome of in-hospital mortality and the secondary outcomes of length of stay and total hospitalization cost for patients with and without DVT or PE. Data was analyzed using descriptive statistics and inferential statistics. Multivariate logistic regression analysis was performed to identify associations of in-hospital mortality. Statistical analysis was conducted using JMP Pro (version 17.0.0, SAS Institute Inc., Cary NC).
Results: A total of 258,333 patients had a diagnosis of acute pancreatitis, with 1,598 (0.62%) having either PE, DVT, or both. The mean age of patients with thromboembolic disease and acute pancreatitis was 59.44 ± 16.15 years, and most patients were male (55.79%) and White (66.19%). Patients with thromboembolic disease have a higher in-hospital mortality rate of 11.90 versus 1.96, p < 0.0001. Amongst minorities, Blacks had the highest rate of mortality (24.86%), followed by Hispanics (10.81) but these differences were not statistically significant, p = 0.2866. Length of stay was also longer for those with DVT or PE, 15.19 days compared to 5.35 days, p= < 0.0001. The total hospitalization cost was almost 3.6 times higher in patients with DVT or PE $205,120.55 compared to $56,805.41, p < 0.0001. Multiple logistic regression analysis showed that DVT or PE was a significant predictor of mortality (OR 12.91, 95% CI 12.05-13.83, p < 0.0001). The strongest predictors of in-hospital mortality were acute kidney injury (OR 16.07, 95% CI 5.68-45.43, p < 0.0001), and severe sepsis with shock (OR 5.58, 95% CI 5.09-6.12, p < 0.0001).
Discussion: Patients with thromboembolic disease and acute pancreatitis are at higher risk for in-hospital mortality and complications. Early detection and aggressive management of deep vein thrombosis or pulmonary emboli in acute pancreatitis can reduce in-hospital mortality.
Disclosures:
Sheena Bhushan, MD1, Riaz Mahmood, MD1, Shane Robinson, MS2, Nikki Nikzad, MS3, Aja McCutchen, MD4. P3430 - Hospitalization Outcomes and Mortality Trends Among Patients With Thromboembolic Disease in Acute Pancreatitis: A Nationwide Inpatient Sample Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Northeast Georgia Medical Center, Buford, GA; 2Northeast Georgia Medical Center, Gainesville, GA; 3Liver Institute Northwest, Seattle, WA; 4Atlanta Gastroenterology Associates, Atlanta, GA
Introduction: There is limited research evaluating outcomes of patients with acute pancreatitis and thromboembolic disease. This study aims to evaluate the influence of deep vein thrombosis (DVT) or pulmonary emboli (PE) on the outcomes of patients presenting with acute pancreatitis utilizing the National Inpatient Sample (NIS) database from 2016 to 2018.
Methods: We performed a retrospective analysis of the NIS database from 2016 to 2018 to identify patients with an acute pancreatitis diagnosis (ICD-10-CM code K85.0-K85.9). We compared the primary outcome of in-hospital mortality and the secondary outcomes of length of stay and total hospitalization cost for patients with and without DVT or PE. Data was analyzed using descriptive statistics and inferential statistics. Multivariate logistic regression analysis was performed to identify associations of in-hospital mortality. Statistical analysis was conducted using JMP Pro (version 17.0.0, SAS Institute Inc., Cary NC).
Results: A total of 258,333 patients had a diagnosis of acute pancreatitis, with 1,598 (0.62%) having either PE, DVT, or both. The mean age of patients with thromboembolic disease and acute pancreatitis was 59.44 ± 16.15 years, and most patients were male (55.79%) and White (66.19%). Patients with thromboembolic disease have a higher in-hospital mortality rate of 11.90 versus 1.96, p < 0.0001. Amongst minorities, Blacks had the highest rate of mortality (24.86%), followed by Hispanics (10.81) but these differences were not statistically significant, p = 0.2866. Length of stay was also longer for those with DVT or PE, 15.19 days compared to 5.35 days, p= < 0.0001. The total hospitalization cost was almost 3.6 times higher in patients with DVT or PE $205,120.55 compared to $56,805.41, p < 0.0001. Multiple logistic regression analysis showed that DVT or PE was a significant predictor of mortality (OR 12.91, 95% CI 12.05-13.83, p < 0.0001). The strongest predictors of in-hospital mortality were acute kidney injury (OR 16.07, 95% CI 5.68-45.43, p < 0.0001), and severe sepsis with shock (OR 5.58, 95% CI 5.09-6.12, p < 0.0001).
Discussion: Patients with thromboembolic disease and acute pancreatitis are at higher risk for in-hospital mortality and complications. Early detection and aggressive management of deep vein thrombosis or pulmonary emboli in acute pancreatitis can reduce in-hospital mortality.
Disclosures:
Sheena Bhushan indicated no relevant financial relationships.
Riaz Mahmood indicated no relevant financial relationships.
Shane Robinson indicated no relevant financial relationships.
Nikki Nikzad indicated no relevant financial relationships.
Aja McCutchen indicated no relevant financial relationships.
Sheena Bhushan, MD1, Riaz Mahmood, MD1, Shane Robinson, MS2, Nikki Nikzad, MS3, Aja McCutchen, MD4. P3430 - Hospitalization Outcomes and Mortality Trends Among Patients With Thromboembolic Disease in Acute Pancreatitis: A Nationwide Inpatient Sample Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
