Tuesday Poster Session
Category: Biliary/Pancreas
P3436 - Gender, Ethnicity, and Vitamin D Deficiency as Potential Predictors of PBC-Related Short-Term and Long-Term Outcomes
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Miriam Sanchez Luna, MD
Texas Health Resources HEB/ Denton
Bedford, TX
Presenting Author(s)
Miriam Sanchez Luna, MD1, Chris Sabillon, MSc2, Angelin Raju, MD3, Carolina DeLaPorte, MD1, Jay Yepuri, MD, FACG4, Marlyn J. Mayo, MD, FACG5
1Texas Health Resources HEB/ Denton, Bedford, TX; 2University of Texas Austin, Northlake, TX; 3Texas Health Resources HEB/Denton, Lewisville, TX; 4Digestive Health Associates of Texas/GI Alliance, Bedford, TX; 5University of Texas Southwestern, Dallas, TX
Introduction: Primary biliary cholangitis (PBC), is an autoimmune disease that progressively destroys the intrahepatic bile ducts. Complications of PBC include malabsorption of fat-soluble vitamins and cirrhosis, which can lead to outcomes such as decompensated cirrhosis, LT, and death. This study aims to establish the association between gender, ethnicity, and vitamin D deficiency in short and long term outcomes for patients with PBC.
Methods: We conducted a retrospective cross-sectional analysis using 2020-2021 HCUP NIS data, including individuals aged 18 and older with PBC cirrhosis-related ICD-10 codes. Outcomes of interest included decompensated cirrhosis (short-term) and HCC, LT, and death (long-term). We used multivariable logistic regression to calculate odds ratios (OR). Significance was set at p< 0.05.
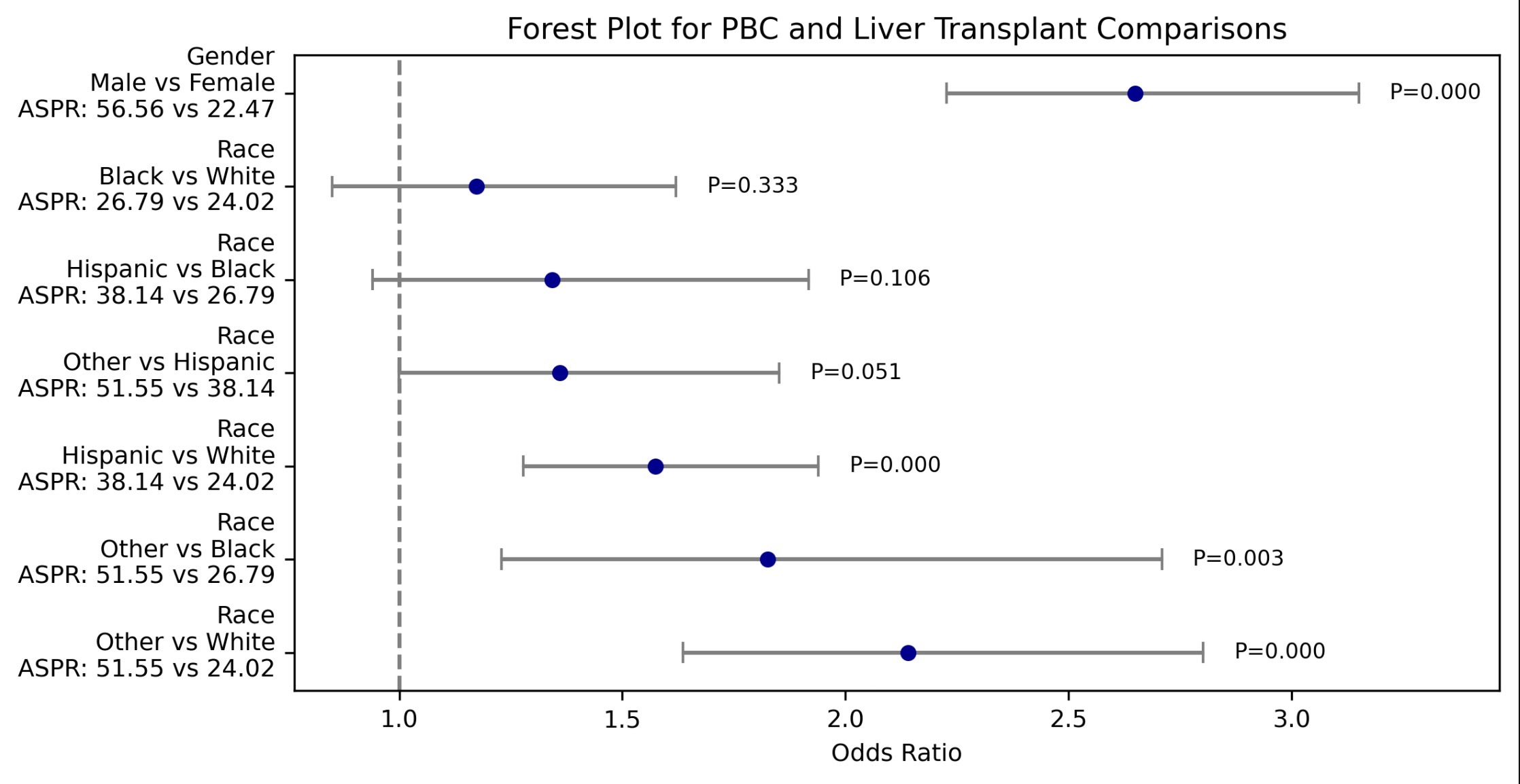
Results: Out of 4873 patients with PBC-related cirrhosis, the median age was 67 years (IQR: 57-76). The median length of stay was 4 days. Demographically, 72.60% were White, 14.53% Hispanic, 6.9% Black, and 5.97% other minorities. Regarding gender, 84.03% were female. Regarding PBC-related decompensated cirrhosis, both Hispanic (OR: 1.276, 95% CI: 1.183-1.376, p < 0.001) and Black individuals (OR: 1.261, 95% CI: 1.135-1.402, p< 0.001) were more likely to develop decompensated cirrhosis compared to White individuals. Males were more likely than females to develop decompensated cirrhosis (OR: 1.299, 95% CI: 1.208-1.397, p < 0.001). Regarding death, Black individuals had higher odds of mortality compared to White individuals (OR: 1.316, 95% CI: 1.057-1.638, p=0.014). Hispanic individuals had the highest odds of receiving liver transplantation compared to White individuals (OR: 1.574, 95% CI: 1.278-1.939, p< 0.001). Individuals with Vitamin D deficiency had higher odds of developing HRS (OR: 1.236, 95% CI: 1.041-1.469, p=0.016) and HCC (OR: 1.657, 95% CI: 1.091-2.516, p=0.018).
Discussion: Previous smaller studies have suggested that minorities (Hispanics and Blacks) and males with PBC are more likely to present with more advanced disease. This study confirms this finding in a larger, national cohort. Vitamin D deficiency was associated with higher risk of HRS, further studies are needed to determine the possible role of CKD leading to Vit D deficiency. Vit D has in vitro effects against hepatoma cell proliferation, so deficiency may create a permissive environment for HCC growth.
Disclosures:
Miriam Sanchez Luna, MD1, Chris Sabillon, MSc2, Angelin Raju, MD3, Carolina DeLaPorte, MD1, Jay Yepuri, MD, FACG4, Marlyn J. Mayo, MD, FACG5. P3436 - Gender, Ethnicity, and Vitamin D Deficiency as Potential Predictors of PBC-Related Short-Term and Long-Term Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Texas Health Resources HEB/ Denton, Bedford, TX; 2University of Texas Austin, Northlake, TX; 3Texas Health Resources HEB/Denton, Lewisville, TX; 4Digestive Health Associates of Texas/GI Alliance, Bedford, TX; 5University of Texas Southwestern, Dallas, TX
Introduction: Primary biliary cholangitis (PBC), is an autoimmune disease that progressively destroys the intrahepatic bile ducts. Complications of PBC include malabsorption of fat-soluble vitamins and cirrhosis, which can lead to outcomes such as decompensated cirrhosis, LT, and death. This study aims to establish the association between gender, ethnicity, and vitamin D deficiency in short and long term outcomes for patients with PBC.
Methods: We conducted a retrospective cross-sectional analysis using 2020-2021 HCUP NIS data, including individuals aged 18 and older with PBC cirrhosis-related ICD-10 codes. Outcomes of interest included decompensated cirrhosis (short-term) and HCC, LT, and death (long-term). We used multivariable logistic regression to calculate odds ratios (OR). Significance was set at p< 0.05.
Results: Out of 4873 patients with PBC-related cirrhosis, the median age was 67 years (IQR: 57-76). The median length of stay was 4 days. Demographically, 72.60% were White, 14.53% Hispanic, 6.9% Black, and 5.97% other minorities. Regarding gender, 84.03% were female. Regarding PBC-related decompensated cirrhosis, both Hispanic (OR: 1.276, 95% CI: 1.183-1.376, p < 0.001) and Black individuals (OR: 1.261, 95% CI: 1.135-1.402, p< 0.001) were more likely to develop decompensated cirrhosis compared to White individuals. Males were more likely than females to develop decompensated cirrhosis (OR: 1.299, 95% CI: 1.208-1.397, p < 0.001). Regarding death, Black individuals had higher odds of mortality compared to White individuals (OR: 1.316, 95% CI: 1.057-1.638, p=0.014). Hispanic individuals had the highest odds of receiving liver transplantation compared to White individuals (OR: 1.574, 95% CI: 1.278-1.939, p< 0.001). Individuals with Vitamin D deficiency had higher odds of developing HRS (OR: 1.236, 95% CI: 1.041-1.469, p=0.016) and HCC (OR: 1.657, 95% CI: 1.091-2.516, p=0.018).
Discussion: Previous smaller studies have suggested that minorities (Hispanics and Blacks) and males with PBC are more likely to present with more advanced disease. This study confirms this finding in a larger, national cohort. Vitamin D deficiency was associated with higher risk of HRS, further studies are needed to determine the possible role of CKD leading to Vit D deficiency. Vit D has in vitro effects against hepatoma cell proliferation, so deficiency may create a permissive environment for HCC growth.
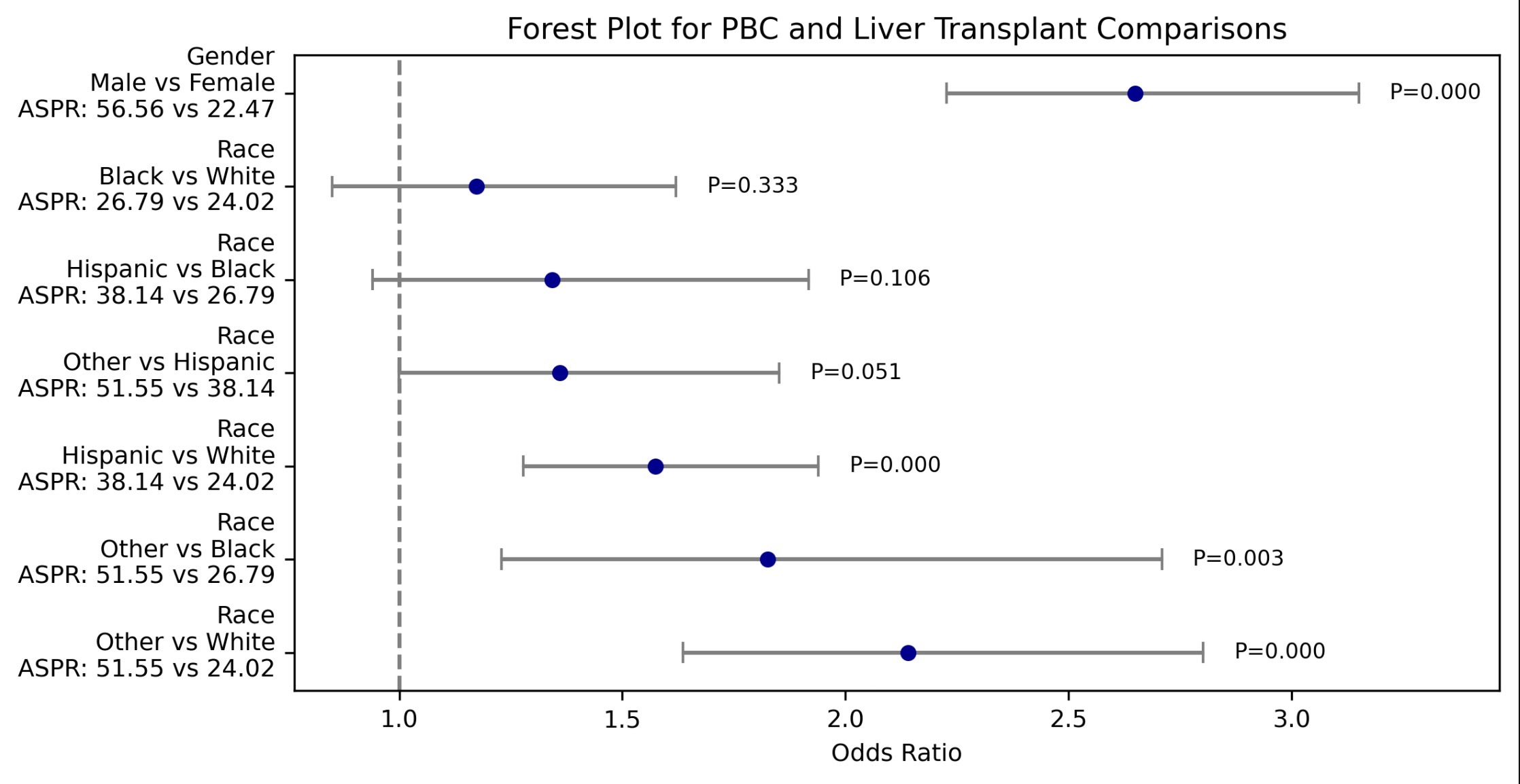
Figure: Forest Plot for PBC and Liver Transplant Comparisons
Disclosures:
Miriam Sanchez Luna indicated no relevant financial relationships.
Chris Sabillon indicated no relevant financial relationships.
Angelin Raju indicated no relevant financial relationships.
Carolina DeLaPorte indicated no relevant financial relationships.
Jay Yepuri indicated no relevant financial relationships.
Marlyn Mayo: CymaBay, a Gilead Sciences Company – Consultant. GSK – Consultant. Intra-Sana – Consultant. Ipsen – Consultant. Mirum – Consultant. Target Pharmasolutions – Consultant.
Miriam Sanchez Luna, MD1, Chris Sabillon, MSc2, Angelin Raju, MD3, Carolina DeLaPorte, MD1, Jay Yepuri, MD, FACG4, Marlyn J. Mayo, MD, FACG5. P3436 - Gender, Ethnicity, and Vitamin D Deficiency as Potential Predictors of PBC-Related Short-Term and Long-Term Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
